Imagine every time you read some text, the letters in between words continually scrambled around. For some people with dyslexia, this is what happens each time they read a book or labels at the grocery store.
Dyslexia is the most common and best-studied of learning disabilities, affecting as many as 15-20% of all people in the U.S. People with dyslexia have a pronounced difficulty with reading despite having standard intelligence, education, and motivation.
Symptoms include trouble with pronunciation, lack of fluency, difficulty retrieving words, poor spelling, and hesitancy in speaking. People with dyslexia might need more time to respond orally to a question and might read more slowly than their peers. Dyslexia is usually diagnosed during elementary school years, when a child is slow to read or struggles with reading. Although reading skills and fluency can improve, dyslexia often persists lifelong.
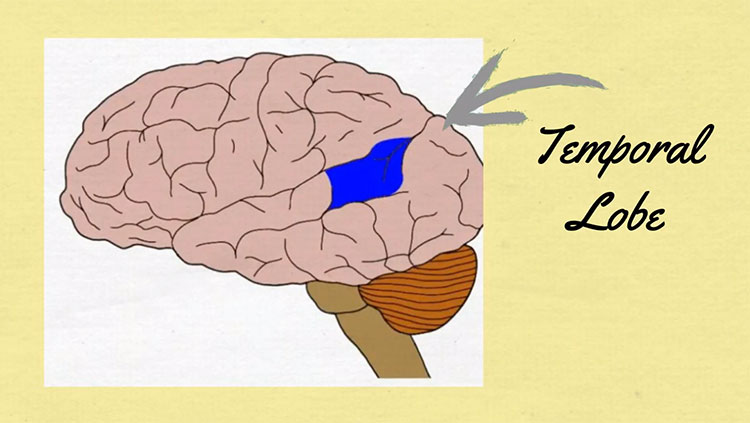
Deciphering printed letters and words, as well as recalling their sounds and meanings, involves many areas of the brain. Brain imaging studies indicate these areas can be less well-connected in people with dyslexia. One of these areas is a region on the left side of the brain called the visual word form area (VWFA), which is involved in the recognition of printed letters and words. People with dyslexia also show less brain activity in the left occipitotemporal cortex, which is considered essential for skilled reading — or fluent execution and coordination of word recognition and text comprehension.
Researchers believe such brain differences are present before the reading and language difficulties become apparent; although another possibility is that people with dyslexia read less and, therefore, their brains develop less in the regions associated with reading. Those with dyslexia also appear to compensate for the reduced activity on the left side of the brain by relying more heavily on the right side.
Genetic analyses have revealed a handful of susceptibility genes, with animal models suggesting these genes affect the migration of brain cells during development, leading to differences in brain circuitry. Dyslexia tends to run in families, with roughly half of those with dyslexia sharing the condition with a close relative. If one twin is diagnosed with dyslexia, the second twin is likely to have the condition 55-70% of the time. But the genetics of dyslexia is complex, and likely involves a wide range of genes and environmental factors.
Treatment for dyslexia involves behavioral and educational intervention, especially exercises like breaking words down into sounds and linking the sounds to specific letter patterns. Some researchers evaluate a child’s ability to name things rapidly and automatically as an early indicator of dyslexia. This rapid automatic naming, and the ability to recognize and work with the sounds of language, are often impaired in people with dyslexia. Both skills can be used in observing preschoolers and kindergartners to predict their later reading skills. Research suggests that treatments targeting phonology, as well as multiple levels of language skills, show the greatest promise.
Adapted from the 8th edition of Brain Facts by Karen Weintraub.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Allen, E. G., Freeman, S. B., Druschel, C., Hobbs, C. A., O'Leary, L. A., Romitti, P. A., Royle, M. H., Torfs, C. P., & Sherman, S. L. (2009). Maternal age and risk for trisomy 21 assessed by the origin of chromosome nondisjunction: a report from the Atlanta and National Down Syndrome Projects. Human genetics, 125(1), 41–52. https://doi.org/10.1007/s00439-008-0603-8
Barbaresi, W. J., Colligan, R. C., Weaver, A. L., Voigt, R. G., Killian, J. M., & Katusic, S. K. (2013). Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics, 131(4), 637–644. https://doi.org/10.1542/peds.2012-2354
Bishop D. V. (2015). The interface between genetics and psychology: lessons from developmental dyslexia. Proceedings. Biological sciences, 282(1806), 20143139. https://doi.org/10.1098/rspb.2014.3139
Casanova, J. R., Nishimura, M., & Swann, J. W. (2014). The effects of early-life seizures on hippocampal dendrite development and later-life learning and memory. Brain research bulletin, 103, 39–48. https://doi.org/10.1016/j.brainresbull.2013.10.004
Casanova, M. (2015). The Neuropathology of Autism. In: Fatemi, S. (eds) The Molecular Basis of Autism. Contemporary Clinical Neuroscience. Springer, New York, NY. 153-171. https://doi.org/10.1007/978-1-4939-2190-4_8
Christensen, D. L., Baio, J., Braun, K. V., Bilder, D., Charles, J., Constantino, J. N., Daniels, J., Maureen, S. Durkin, M. S., Robert, T., Fitzgerald, R. T., Kurzius-Spencer, M., Lee, L., Pettygrove, S., Robinson, C., Schulz, E., Wells, C., Wingate, M. S., Zahorodny, W., Yeargin-Allsopp, M. (2016). Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveill Summ 2016;65(No. SS-3)(No. SS-3):1–23. DOI: http://dx.doi.org/10.15585/mmwr.ss6503a1external icon.
Chronis-Tuscano, A., Molina, B. S., Pelham, W. E., Applegate, B., Dahlke, A., Overmyer, M., & Lahey, B. B. (2010). Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of general psychiatry, 67(10), 1044–1051. https://doi.org/10.1001/archgenpsychiatry.2010.127
Durkin, M. S., Maenner, M. J., Newschaffer, C. J., Lee, L. C., Cunniff, C. M., Daniels, J. L., Kirby, R. S., Leavitt, L., Miller, L., Zahorodny, W., & Schieve, L. A. (2008). Advanced parental age and the risk of autism spectrum disorder. American journal of epidemiology, 168(11), 1268–1276. https://doi.org/10.1093/aje/kwn250
Emerson, R. W., Adams, C., Nishino, T., Hazlett, H. C., Wolff, J. J., Zwaigenbaum, L., Constantino, J. N., Shen, M. D., Swanson, M. R., Elison, J. T., Kandala, S., Estes, A. M., Botteron, K. N., Collins, L., Dager, S. R., Evans, A. C., Gerig, G., Gu, H., McKinstry, R. C., Paterson, S., … Piven, J. (2017). Functional neuroimaging of high-risk 6-month-old infants predicts a diagnosis of autism at 24 months of age. Science translational medicine, 9(393), eaag2882. https://doi.org/10.1126/scitranslmed.aag2882
Finn, E. S., Shen, X., Holahan, J. M., Scheinost, D., Lacadie, C., Papademetris, X., Shaywitz, S. E., Shaywitz, B. A., & Constable, R. T. (2014). Disruption of functional networks in dyslexia: a whole-brain, data-driven analysis of connectivity. Biological psychiatry, 76(5), 397–404. https://doi.org/10.1016/j.biopsych.2013.08.031
Fisch, H., Hyun, G., Golden, R., Hensle, T. W., Olsson, C. A., & Liberson, G. L. (2003). The influence of paternal age on down syndrome. The Journal of urology, 169(6), 2275–2278. https://doi.org/10.1097/01.ju.0000067958.36077.d8
Frazier, T. W., Klingemier, E. W., Beukemann, M., Speer, L., Markowitz, L., Parikh, S., Wexberg, S., Giuliano, K., Schulte, E., Delahunty, C., Ahuja, V., Eng, C., Manos, M. J., Hardan, A. Y., Youngstrom, E. A., & Strauss, M. S. (2016). Development of an Objective Autism Risk Index Using Remote Eye Tracking. Journal of the American Academy of Child and Adolescent Psychiatry, 55(4), 301–309. https://doi.org/10.1016/j.jaac.2016.01.011
Geschwind, D. H., & State, M. W. (2015). Gene hunting in autism spectrum disorder: on the path to precision medicine. The Lancet. Neurology, 14(11), 1109–1120. https://doi.org/10.1016/S1474-4422(15)00044-7
Guastella, A. J., & Hickie, I. B. (2016). Oxytocin Treatment, Circuitry, and Autism: A Critical Review of the Literature Placing Oxytocin Into the Autism Context. Biological psychiatry, 79(3), 234–242. https://doi.org/10.1016/j.biopsych.2015.06.028
Hallmayer, J., Cleveland, S., Torres, A., et al. Genetic Heritability and Shared Environmental Factors Among Twin Pairs With Autism. Arch Gen Psychiatry. 2011;68(11):1095–1102. doi:10.1001/archgenpsychiatry.2011.76
Helguera, P., Seiglie, J., Rodriguez, J., Hanna, M., Helguera, G., & Busciglio, J. (2013). Adaptive downregulation of mitochondrial function in down syndrome. Cell metabolism, 17(1), 132–140. https://doi.org/10.1016/j.cmet.2012.12.005
Hornig, M., Bresnahan, M. A., Che, X., Schultz, A. F., Ukaigwe, J. E., Eddy, M. L., Hirtz, D., Gunnes, N., Lie, K. K., Magnus, P., Mjaaland, S., Reichborn-Kjennerud, T., Schjølberg, S., Øyen, A. S., Levin, B., Susser, E. S., Stoltenberg, C., & Lipkin, W. I. (2018). Prenatal fever and autism risk. Molecular psychiatry, 23(3), 759–766. https://doi.org/10.1038/mp.2017.119
Jiang, J., Jing, Y., Cost, G. J., Chiang, J. C., Kolpa, H. J., Cotton, A. M., Carone, D. M., Carone, B. R., Shivak, D. A., Guschin, D. Y., Pearl, J. R., Rebar, E. J., Byron, M., Gregory, P. D., Brown, C. J., Urnov, F. D., Hall, L. L., & Lawrence, J. B. (2013). Translating dosage compensation to trisomy 21. Nature, 500(7462), 296–300. https://doi.org/10.1038/nature12394
Kasparek, T., Theiner, P., & Filova, A. (2015). Neurobiology of ADHD From Childhood to Adulthood: Findings of Imaging Methods. Journal of attention disorders, 19(11), 931–943. https://doi.org/10.1177/1087054713505322
Katsnelson, A., Buzsáki, G., & Swann, J. W. (2014). Catastrophic childhood epilepsy: a recent convergence of basic and clinical neuroscience. Science translational medicine, 6(262), 262ps13.
Kozlowski, A. M., Matson, J. L., Horovitz, M., Worley, J. A., & Neal, D. (2011). Parents' first concerns of their child's development in toddlers with autism spectrum disorders. Developmental neurorehabilitation, 14(2), 72–78. https://doi.org/10.3109/17518423.2010.539193
Lainhart J. E. (2015). Brain imaging research in autism spectrum disorders: in search of neuropathology and health across the lifespan. Current opinion in psychiatry, 28(2), 76–82. https://doi.org/10.1097/YCO.0000000000000130
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thurm, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of general psychiatry, 63(6), 694–701. https://doi.org/10.1001/archpsyc.63.6.694
National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. (2016). Autism Spectrum Disorder (ASD): Data & Statistics. Centers for Disease Control. https://www.cdc.gov/autism/data-research/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/autism/data.html
Nei, M., Ngo, L., Sirven, J. I., & Sperling, M. R. (2014). Ketogenic diet in adolescents and adults with epilepsy. Seizure, 23(6), 439–442. https://doi.org/10.1016/j.seizure.2014.02.015
Norton, E. S., & Wolf, M. (2012). Rapid automatized naming (RAN) and reading fluency: implications for understanding and treatment of reading disabilities. Annual review of psychology, 63, 427–452. https://doi.org/10.1146/annurev-psych-120710-100431
Ozernov-Palchik, O., & Gaab, N. (2016). Tackling the 'dyslexia paradox': reading brain and behavior for early markers of developmental dyslexia. Wiley interdisciplinary reviews. Cognitive science, 7(2), 156–176. https://doi.org/10.1002/wcs.1383
Ozonoff, S., Young, G. S., Carter, A., Messinger, D., Yirmiya, N., Zwaigenbaum, L., Bryson, S., Carver, L. J., Constantino, J. N., Dobkins, K., Hutman, T., Iverson, J. M., Landa, R., Rogers, S. J., Sigman, M., & Stone, W. L. (2011). Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics, 128(3), e488–e495. https://doi.org/10.1542/peds.2010-2825
Papavassiliou, P., Charalsawadi, C., Rafferty, K., & Jackson-Cook, C. (2015). Mosaicism for trisomy 21: a review. American journal of medical genetics. Part A, 167A(1), 26–39. https://doi.org/10.1002/ajmg.a.36861
Paulesu, E., Danelli, L., & Berlingeri, M. (2014). Reading the dyslexic brain: multiple dysfunctional routes revealed by a new meta-analysis of PET and fMRI activation studies. Frontiers in human neuroscience, 8, 830. https://doi.org/10.3389/fnhum.2014.00830
Presson, A. P., Partyka, G., Jensen, K. M., Devine, O. J., Rasmussen, S. A., McCabe, L. L., & McCabe, E. R. (2013). Current estimate of Down Syndrome population prevalence in the United States. The Journal of pediatrics, 163(4), 1163–1168. https://doi.org/10.1016/j.jpeds.2013.06.013
Schendel, D., & Bhasin, T. K. (2008). Birth weight and gestational age characteristics of children with autism, including a comparison with other developmental disabilities. Pediatrics, 121(6), 1155–1164. https://doi.org/10.1542/peds.2007-1049
Thapar, A., Cooper, M., Eyre, O., & Langley, K. (2013). What have we learnt about the causes of ADHD?. Journal of child psychology and psychiatry, and allied disciplines, 54(1), 3–16. https://doi.org/10.1111/j.1469-7610.2012.02611.x
Tolaymat, A., Nayak, A., Geyer, J. D., Geyer, S. K., & Carney, P. R. (2015). Diagnosis and management of childhood epilepsy. Current problems in pediatric and adolescent health care, 45(1), 3–17. https://doi.org/10.1016/j.cppeds.2014.12.002
Tomasi, D., & Volkow, N. D. (2014). Functional connectivity of substantia nigra and ventral tegmental area: maturation during adolescence and effects of ADHD. Cerebral cortex (New York, N.Y. : 1991), 24(4), 935–944. https://doi.org/10.1093/cercor/bhs382
Visser, S. N., Danielson, M. L., Bitsko, R. H., Holbrook, J. R., Kogan, M. D., Ghandour, R. M., Perou, R., & Blumberg, S. J. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. Journal of the American Academy of Child and Adolescent Psychiatry, 53(1), 34–46.e2. https://doi.org/10.1016/j.jaac.2013.09.001
Willsey, A. J., & State, M. W. (2015). Autism spectrum disorders: from genes to neurobiology. Current opinion in neurobiology, 30, 92–99. https://doi.org/10.1016/j.conb.2014.10.015
Wiseman, F. K., Al-Janabi, T., Hardy, J., Karmiloff-Smith, A., Nizetic, D., Tybulewicz, V. L., Fisher, E. M., & Strydom, A. (2015). A genetic cause of Alzheimer disease: mechanistic insights from Down syndrome. Nature reviews. Neuroscience, 16(9), 564–574. https://doi.org/10.1038/nrn3983
Witton, J., Padmashri, R., Zinyuk, L. E., Popov, V. I., Kraev, I., Line, S. J., Jensen, T. P., Tedoldi, A., Cummings, D. M., Tybulewicz, V. L. J., Fisher, E. M. C., Bannerman, D. M., Randall, A. D., Brown, J. T., Edwards, F. A., Rusakov, D. A., Stewart, M. G., & Jones, M. W. (2015). Hippocampal circuit dysfunction in the Tc1 mouse model of Down syndrome. Nature neuroscience, 18(9), 1291–1298. https://doi.org/10.1038/nn.4072
Young, L. J., & Barrett, C. E. (2015). Neuroscience. Can oxytocin treat autism? Science (New York, N.Y.), 347(6224), 825–826. https://doi.org/10.1126/science.aaa8120
Zuberi, S. M., & Symonds, J. D. (2015). Update on diagnosis and management of childhood epilepsies. Jornal de pediatria, 91(6 Suppl 1), S67–S77. https://doi.org/10.1016/j.jped.2015.07.003
What to Read Next
Also In Language
Trending
Popular articles on BrainFacts.org