How Sleep Changes Could Serve as an Early Alzheimer’s Biomarker
- Published29 Oct 2024
- Author Bella Isaacs-Thomas
- Source BrainFacts/SfN

People with Alzheimer’s are diagnosed based on evidence they’re experiencing cognitive decline. However, symptoms like memory issues or behavioral changes emerge far into the disease’s progression, which means most patients have already endured significant brain damage once they receive an official diagnosis.
That’s why researchers are searching for biomarkers — measurable physiological cues which could point to Alzheimer’s before more obvious symptoms are in full swing. New preliminary findings presented at Neuroscience 2024 in Chicago, the Society for Neuroscience’s annual meeting, shed light on how specific sleep patterns could be an early indicator of the disease.
Sleep is crucial for maintaining brain health, and poor sleep can even increase a person’s risk of dementia. However, around a third of adults in the United States aren’t getting their recommended seven hours of sleep per night, according to the Centers for Disease Control and Prevention. People with Alzheimer’s are particularly likely to grapple with a variety of challenges to getting sufficient sleep.
A new study spearheaded by Florida State University graduate student Emily Salvador used rodent models to examine the link between sleep and Alzheimer’s. Aaron Wilber, associate professor in Florida State University’s department of psychology, presented their team’s work.
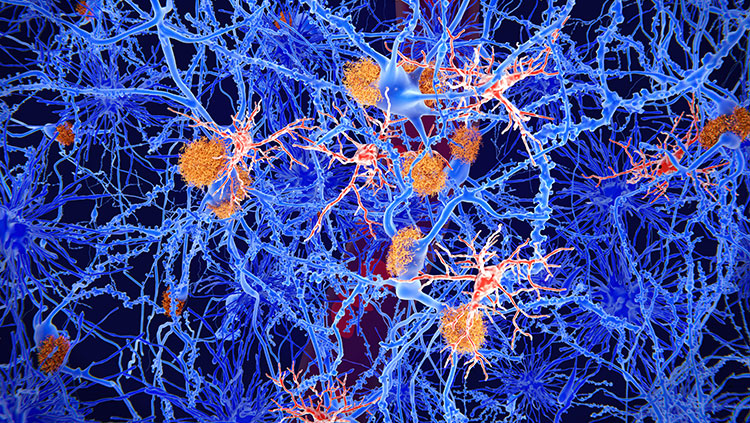
The rats and mice involved in their research were genetically altered so that their brains mirrored Alzheimer’s disease progression in a human brain. People with Alzheimer’s have a buildup of amyloid beta plaques and tau proteins. In healthy brains, amyloid beta production decreases during sleep, Wilber said.
To assess brain health in those rodent models, the researchers analyzed delta and theta brain rhythms, brain states associated with deep sleep and the relaxed phase just before sleep. They found the rodents representing early Alzheimer’s disease experienced shallower sleep compared to healthy ones, even as they slept for longer periods of time.
Wilber said assessing those brain waves in humans could offer clues as to whether a person may be on track to receive an Alzheimer’s diagnosis. “These early sleep changes could serve as a potential early biomarker for Alzheimer's disease, and potentially a sign [for] when you want to implement preventative treatments,” Wilber said.
Beyond its potential role as a biomarker, tracking early sleep disturbances earlier could also allow health care providers more time to intervene and potentially remove barriers for patients who struggle with sleep.
Experts believe harmful proteins are still present before they become measurable in Alzheimer’s disease patients, and they can disrupt brain function in more subtle ways — including, potentially, by disrupting sleep, said Bryce Mander, assistant professor of psychiatry and human behavior at University of California, Irvine.
An intricate web of factors influences brain health across a person’s life, and they become even more consequential as they age. Mander noted health challenges like inflammation, sleep apnea, and stress can lead to poor sleep, and even when they’re not directly related to Alzheimer’s, they can influence how the disease plays out in patients.
“Alzheimer’s disease is more complicated than sleep, and sleep is only one contributing component, but it might be something you can do something about,” Mander said.
Still, evidence suggests early sleep interventions can play a meaningful role in improving outcomes. Mander pointed to research involving sleep apnea, a risk factor for dementia associated with an earlier average age of onset. He pointed to one study in which people who received quality treatment to resolve sleep apnea no longer had a higher risk for earlier dementia onset.
“The idea behind it is you have a sleep disorder that is impacting risk — sleep is modifiable,” Mander said. “You target that sleep treatment, you might remove the sleep contribution to that risk. And that in itself can have a profound impact.”
CONTENT PROVIDED BY
BrainFacts/SfN
References
What to Read Next
Also In Alzheimer's & Dementia
Trending
Popular articles on BrainFacts.org


.jpg)