Suffering and Recovering from a Stroke
- Reviewed28 Aug 2023
- Author Gail Zyla
- Source BrainFacts/SfN

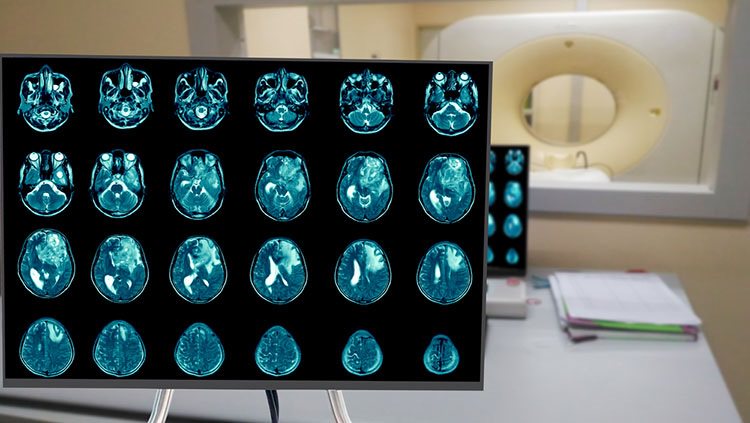
Like the rest of your body, your brain requires a steady flow of oxygen and glucose-rich blood for it to function. When the blood flow to one area is interrupted or blocked, brain cells can start to die within minutes.
Each year, nearly 800,000 people in the United States suffer a stroke — an interruption in blood flow to the brain due to a ruptured blood vessel or a blood clot. Of these, about 600,000 are first-time strokes. Strokes are a leading cause of long-term disability in the United States, costing about *$56.5 billion each year, including the costs of health care services and medicines to treat stroke, and missed days of work.
Risk factors for stroke include older age, high blood pressure, atrial fibrillation, heart disease, high cholesterol, diabetes, physical inactivity, obesity, smoking, and drinking too much alcohol. Controlling these factors by maintaining a healthful weight, exercising, avoiding excessive alcohol intake, and taking medications for stroke-related physical problems can reduce the risk of having a stroke. There is also a genetic risk for stroke, especially evident if there is a parental history of stroke. To date, several candidate genes have been suggested, but increased stroke risk is most likely due to multiple genetic factors. There are also well-defined genetic risks of stroke such a sickle cell disease.
There are various types of strokes. Ischemic strokes occur when a blood vessel supplying blood to the brain clots. These account for 87% of all strokes. These strokes can occur due to a buildup of cholesterol in the blood vessel wall or a detachment of a clot from the carotid arteries (major blood vessels that provide your brain's blood supply) or the heart, lodging itself into a blood vessel in your brain. A transient ischemic attack (TIA) is a temporary blockage of blood flow to the brain, which usually gets dislodged or dissolves on its own with symptoms that usually last up to a day or less. This “warning stroke” signals a possible full-blown stroke ahead. Hemorrhagic strokes occur when a weakened blood vessel ruptures and bleeds into the brain. All these causes of strokes are serious medical conditions that require emergency care as quickly as possible to prevent further brain damage or death.
The acronym B.E.F.A.S.T. can be used to help people identify and act on the early warning signs of a stroke. B.E.F.A.S.T. stands for:
- Balance (a sudden loss of balance or coordination, or onset of dizziness)
- Eyes (a sudden difficulty seeing out of one or both eyes)
- Face (asymmetry or numbness in the face)
- Arms (weakness or numbness in the arms)
- Speech (slurred or garbled speech)
- Time (call emergency services if any of the above signs are present)
Until recently, treatments for a stroke did not go far beyond physical or speech therapy. Today, however, clot-dissolving medications known as thrombolytics are a standard treatment. Tissue plasminogen activator (tPA), a clot-dissolving drug approved by the FDA in 1996, helps to break down blood clots and open blocked blood vessels. tPA can restore circulation before oxygen and glucose loss causes permanent brain damage; given within three hours of a stroke, its use often limits brain damage. Tenecteplase (TNK), another thrombolytic not FDA approved for stroke treatment, has been used in clinical trials to test its effectiveness as an alternative thrombolytic. Anticoagulant drugs given to patients with stroke risk factors help by reducing the likelihood of clots forming in the heart or arteries and traveling to the brain, causing a stroke. In addition, major advances in surgery has shown success in opening clogged arteries, and treatments targeting heart problems like atrial fibrillation can help prevent strokes.
Strokes have a range of long-term outcomes: paralysis, weakness, numbness, pain, mental health conditions, and trouble with speech, cognition, emotions, and motor skills. Rehabilitation efforts following strokes can include engaging in physical therapy, speech therapy, occupational therapy, and connecting with support groups.
Research is underway to find new methods for preventing and treating strokes. Some drugs have been shown to be effective at preventing damage to the nervous system, including nerve cell death following a stroke. Another promising research area is the use of neural stem cells to improve recovery after a stroke. Preliminary research suggests that injection of stem cells helps promote recovery, even when given several days after a stroke. Administering growth-stimulating substances along with the stem cells might enhance the benefits of stem cell transplant.
Adapted from the 8th edition of Brain Facts by Gail Zyla.
*This number has been updated to reflect the latest estimates for stroke’s cost of illness in the United States.
CONTENT PROVIDED BY
BrainFacts/SfN
References
American Stroke Association. (2023). Types of Stroke and Treatment. https://www.stroke.org/en/about-stroke/types-of-stroke
Bang, O. Y., Kim, E. H., Cha, J. M., & Moon, G. J. (2016). Adult Stem Cell Therapy for Stroke: Challenges and Progress. Journal of stroke, 18(3), 256–266. https://doi.org/10.5853/jos.2016.01263
Centers for Disease Control and Prevention. (2017). HIV in the United States and Dependent Areas. https://www.cdc.gov/hiv/statistics/overview/ataglance.html
Centers for Disease Control and Prevention. (2017). Stroke Facts. https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2017). Traumatic Brain Injury & Concussion. https://www.cdc.gov/TraumaticBrainInjury/
Chapman, S. N., Mehndiratta, P., Johansen, M. C., McMurry, T. L., Johnston, K. C., & Southerland, A. M. (2014). Current perspectives on the use of intravenous recombinant tissue plasminogen activator (tPA) for treatment of acute ischemic stroke. Vascular health and risk management, 10, 75–87. https://doi.org/10.2147/VHRM.S39213
Correale, J., Gaitán, M. I., Ysrraelit, M. C., & Fiol, M. P. (2017). Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain : a journal of neurology, 140(3), 527–546. https://doi.org/10.1093/brain/aww258
Doulames, V. M., & Plant, G. W. (2016). Induced Pluripotent Stem Cell Therapies for Cervical Spinal Cord Injury. International journal of molecular sciences, 17(4), 530. https://doi.org/10.3390/ijms17040530
Gereau, R. W., 4th, Sluka, K. A., Maixner, W., Savage, S. R., Price, T. J., Murinson, B. B., Sullivan, M. D., & Fillingim, R. B. (2014). A pain research agenda for the 21st century. The journal of pain, 15(12), 1203–1214. https://doi.org/10.1016/j.jpain.2014.09.004
Krieger S. C. (2016). New Approaches to the Diagnosis, Clinical Course, and Goals of Therapy in Multiple Sclerosis and Related Disorders. Continuum (Minneapolis, Minn.), 22(3), 723–729. https://doi.org/10.1212/CON.0000000000000324
Martucci, K. T., Ng, P., & Mackey, S. (2014). Neuroimaging chronic pain: what have we learned and where are we going?. Future neurology, 9(6), 615–626. https://doi.org/10.2217/FNL.14.57
Matinella, A., Lanzafame, M., Bonometti, M. A., Gajofatto, A., Concia, E., Vento, S., Monaco, S., & Ferrari, S. (2015). Neurological complications of HIV infection in pre-HAART and HAART era: a retrospective study. Journal of neurology, 262(5), 1317–1327. https://doi.org/10.1007/s00415-015-7713-8
National Brain Tumor Society. (2023). Brain Tumor Facts. Brain Tumors. https://braintumor.org/brain-tumors/about-brain-tumors/brain-tumor-facts/
National Cancer Institute. (2017). Cancer Stat Facts: Brain and Other Nervous System Cancer. NIH. https://seer.cancer.gov/statfacts/html/brain.html
National Cancer Institute. (2023). Brain Tumor. NCI Dictionary of Cancer Terms. NIH. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/brain-tumor
National Spinal Cord Injury Statistical Center. (2017). University of Alabama at Birmingham. https://www.nscisc.uab.edu/
Okura, H., Smith, C. A., & Rutka, J. T. (2014). Gene therapy for malignant glioma. Molecular and cellular therapies, 2, 21. https://doi.org/10.1186/2052-8426-2-21
Reardon, D. A., Freeman, G., Wu, C., Chiocca, E. A., Wucherpfennig, K. W., Wen, P. Y., Fritsch, E. F., Curry, W. T., Jr, Sampson, J. H., & Dranoff, G. (2014). Immunotherapy advances for glioblastoma. Neuro-oncology, 16(11), 1441–1458. https://doi.org/10.1093/neuonc/nou212
Rosado, I. R., Lavor, M. S., Alves, E. G., Fukushima, F. B., Oliveira, K. M., Silva, C. M., Caldeira, F. M., Costa, P. M., & Melo, E. G. (2014). Effects of methylprednisolone, dantrolene, and their combination on experimental spinal cord injury. International journal of clinical and experimental pathology, 7(8), 4617–4626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152024/
Schonberg, D. L., Lubelski, D., Miller, T. E., & Rich, J. N. (2014). Brain tumor stem cells: Molecular characteristics and their impact on therapy. Molecular aspects of medicine, 39, 82–101. https://doi.org/10.1016/j.mam.2013.06.004
Schulenburg, A., Blatt, K., Cerny-Reiterer, S., Sadovnik, I., Herrmann, H., Marian, B., Grunt, T. W., Zielinski, C. C., & Valent, P. (2015). Cancer stem cells in basic science and in translational oncology: can we translate into clinical application?. Journal of hematology & oncology, 8, 16. https://doi.org/10.1186/s13045-015-0113-9
Simons, L. E., & Basch, M. C. (2016). State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain management, 6(1), 49–61. https://doi.org/10.2217/pmt.15.59
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: a neural systems approach. Neuroscience and biobehavioral reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Stuckey, D. W., & Shah, K. (2014). Stem cell-based therapies for cancer treatment: separating hope from hype. Nature reviews. Cancer, 14(10), 683–691. https://doi.org/10.1038/nrc3798
Su, Y. S., Ali, R., Feroze, A. H., Li, G., Lawton, M. T., & Choudhri, O. (2016). Endovascular therapies for malignant gliomas: Challenges and the future. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 26, 26–32. https://doi.org/10.1016/j.jocn.2015.10.019
Understanding the HIV Epidemic. (2017). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/data
Wang, S. X., Ho, E. L., Grill, M., Lee, E., Peterson, J., Robertson, K., Fuchs, D., Sinclair, E., Price, R. W., & Spudich, S. (2014). Peripheral neuropathy in primary HIV infection associates with systemic and central nervous system immune activation. Journal of acquired immune deficiency syndromes (1999), 66(3), 303–310. https://doi.org/10.1097/QAI.0000000000000167
White, H. & Venkatesh, B. (2016). Traumatic brain injury. Oxford Textbook of Neurocritical Care, 17. https://books.google.com/books?hl=en&lr=&id=o7hlCwAAQBAJ&oi=fnd&pg=PA210&dq=traumatic+brain+injury&ots=53PDiF2Jhx&sig=TPqEUTtTpGBJdRxBbZPcgO1pqpc#v=onepage&q=traumatic%20brain%20injury&f=false
What to Read Next
Also In Injury
Trending
Popular articles on BrainFacts.org