Glimpses into Spinal Cord Injury
- Reviewed14 Aug 2023
- Author Gail Zyla
- Source BrainFacts/SfN

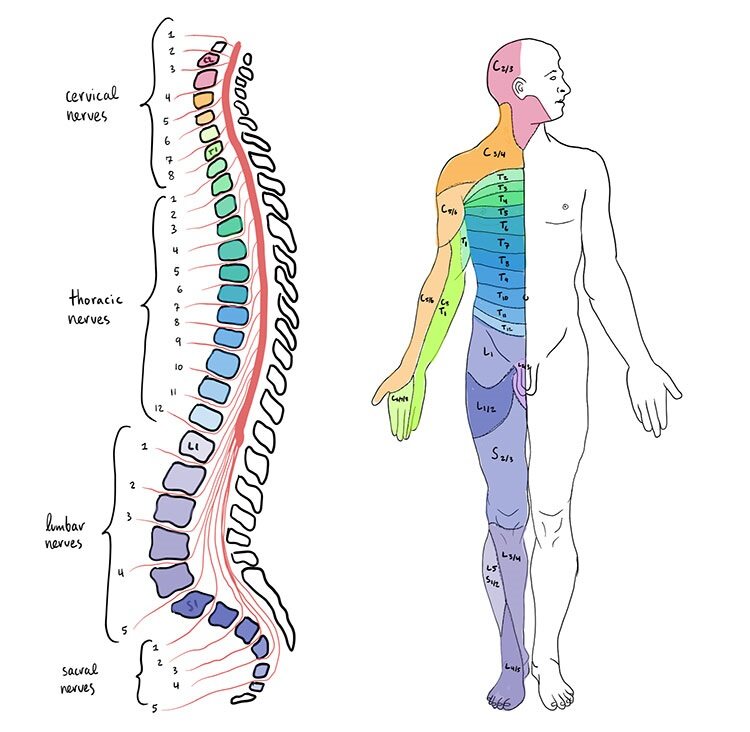
Our spinal cords often take a back seat to the brain when we think of our central nervous system. But this vital bundle of nervous system tissue — protected by the vertebral column running down our backs — gives us the ability to communicate with our bodies. Injury to the spinal cord can have ranging impacts on mobility, bodily control, and bodily sensation.
A spinal cord injury (SCI) disrupts the neural architecture that carries information along the spinal cord and results in a loss of functions. SCIs can occur when a sudden, traumatic blow to the spine fractures or dislocates vertebrae, destroying nerve cells that carry signals along the spinal cord. SCIs also can arise from other non-traumatic forces, like from tumors, demyelinating conditions, blood clots, strokes, and more. Each year, about 17,000 people suffer spinal cord injuries in the United States, and an estimated 282,000 people in the U.S. currently live with spinal cord injuries.
Vehicle crashes are the leading cause of spinal cord injuries, followed by falls, acts of violence (primarily gunshot wounds), and injuries from contact sports and recreational activities. No two spinal cord injuries are the same. SCIs can vary in their damaging impacts depending on the severity of injury and where along the spinal cord the injury occurs, leading to different outcomes. Death rates among people with spinal cord injuries are significantly higher during the first year after the injury, especially people whose injuries cause severe neurological impairments.
There are currently no FDA approved remedies to prevent or repair neurological damage incurred by injuries to the spinal cord; however, some methods like spine realignment and stabilization and surgery are standard practice to help limit the damage that develops after the initial injury. In addition, there are ongoing efforts to support better rehabilitation techniques, as well as research into repairing and regenerating injured tissue and nerve cells to restore communication.
SCIs can permanently damage nerve cells and cause a wide range of disabilities — including various degrees of paralysis. *Pregabalin, an anticonvulsant and pain reliever, can help with the management of neuropathic pain commonly experienced following a SCI. But there are no drugs or treatment approaches yet approved to restore function following a SCI. Other future treatment candidates aim to assist nerve regrowth after the injury.
There is no cure for spinal cord injuries, but scientists are investigating new ways to repair damaged spinal cords. These include protecting surviving nerve cells from further damage, replacing damaged nerve cells, stimulating the regrowth of axons and targeting their connections, and retraining nerve circuits to restore bodily functions. In addition, scientists constantly search for new methods for rehabilitating patients with SCI and improving their quality of life. Rehabilitation focuses on physical therapy to strengthen muscles and improve mobility. Occupational therapy focuses on enhancing fine motor skills, such as the skills needed to write or type.
Electrical muscle stimulation is sometimes used in the clinic to help restore function to muscles affected by the injury. Scientists have developed experimental procedures to stimulate the spinal cord directly, which has demonstrated promising results for restoring some limited functions lost after spinal cord injury.
Stem cells can be used to repair circuits at the site of injury. These cells grown in the lab, which can be derived from a patient’s own tissues, can develop into different kinds of cell types like other nerve cells — helping them integrate to and repair circuits they are introduced to. Researchers are continuing to understand how certain neurochemical and cellular barriers that prevent regrowth and repair can be overcome and how the newly born cells can be induced to integrate into the injured circuit.
Adapted from the 8th edition of Brain Facts by Gail Zyla.
*This section was updated August 14, 2023, to include information on Pregabalin, a treatment for neuropathic pain associated with SCI.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Bang, O. Y., Kim, E. H., Cha, J. M., & Moon, G. J. (2016). Adult Stem Cell Therapy for Stroke: Challenges and Progress. Journal of stroke, 18(3), 256–266. https://doi.org/10.5853/jos.2016.01263
Centers for Disease Control and Prevention. (2017). HIV in the United States and Dependent Areas. https://www.cdc.gov/hiv/statistics/overview/ataglance.html
Centers for Disease Control and Prevention. (2017). Stroke Facts. https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2017). Traumatic Brain Injury & Concussion. https://www.cdc.gov/TraumaticBrainInjury/
Chapman, S. N., Mehndiratta, P., Johansen, M. C., McMurry, T. L., Johnston, K. C., & Southerland, A. M. (2014). Current perspectives on the use of intravenous recombinant tissue plasminogen activator (tPA) for treatment of acute ischemic stroke. Vascular health and risk management, 10, 75–87. https://doi.org/10.2147/VHRM.S39213
Correale, J., Gaitán, M. I., Ysrraelit, M. C., & Fiol, M. P. (2017). Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain : a journal of neurology, 140(3), 527–546. https://doi.org/10.1093/brain/aww258
Doulames, V. M., & Plant, G. W. (2016). Induced Pluripotent Stem Cell Therapies for Cervical Spinal Cord Injury. International journal of molecular sciences, 17(4), 530. https://doi.org/10.3390/ijms17040530
Gereau, R. W., 4th, Sluka, K. A., Maixner, W., Savage, S. R., Price, T. J., Murinson, B. B., Sullivan, M. D., & Fillingim, R. B. (2014). A pain research agenda for the 21st century. The journal of pain, 15(12), 1203–1214. https://doi.org/10.1016/j.jpain.2014.09.004
Krieger S. C. (2016). New Approaches to the Diagnosis, Clinical Course, and Goals of Therapy in Multiple Sclerosis and Related Disorders. Continuum (Minneapolis, Minn.), 22(3), 723–729. https://doi.org/10.1212/CON.0000000000000324
Martucci, K. T., Ng, P., & Mackey, S. (2014). Neuroimaging chronic pain: what have we learned and where are we going?. Future neurology, 9(6), 615–626. https://doi.org/10.2217/FNL.14.57
Matinella, A., Lanzafame, M., Bonometti, M. A., Gajofatto, A., Concia, E., Vento, S., Monaco, S., & Ferrari, S. (2015). Neurological complications of HIV infection in pre-HAART and HAART era: a retrospective study. Journal of neurology, 262(5), 1317–1327. https://doi.org/10.1007/s00415-015-7713-8
National Brain Tumor Society. (2023). Brain Tumor Facts. Brain Tumors. https://braintumor.org/brain-tumors/about-brain-tumors/brain-tumor-facts/
National Cancer Institute. (2017). Cancer Stat Facts: Brain and Other Nervous System Cancer. NIH. https://seer.cancer.gov/statfacts/html/brain.html
National Cancer Institute. (2023). Brain Tumor. NCI Dictionary of Cancer Terms. NIH. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/brain-tumor
National Spinal Cord Injury Statistical Center. (2017). University of Alabama at Birmingham. https://www.nscisc.uab.edu/
Okura, H., Smith, C. A., & Rutka, J. T. (2014). Gene therapy for malignant glioma. Molecular and cellular therapies, 2, 21. https://doi.org/10.1186/2052-8426-2-21
Reardon, D. A., Freeman, G., Wu, C., Chiocca, E. A., Wucherpfennig, K. W., Wen, P. Y., Fritsch, E. F., Curry, W. T., Jr, Sampson, J. H., & Dranoff, G. (2014). Immunotherapy advances for glioblastoma. Neuro-oncology, 16(11), 1441–1458. https://doi.org/10.1093/neuonc/nou212
Rosado, I. R., Lavor, M. S., Alves, E. G., Fukushima, F. B., Oliveira, K. M., Silva, C. M., Caldeira, F. M., Costa, P. M., & Melo, E. G. (2014). Effects of methylprednisolone, dantrolene, and their combination on experimental spinal cord injury. International journal of clinical and experimental pathology, 7(8), 4617–4626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152024/
Schonberg, D. L., Lubelski, D., Miller, T. E., & Rich, J. N. (2014). Brain tumor stem cells: Molecular characteristics and their impact on therapy. Molecular aspects of medicine, 39, 82–101. https://doi.org/10.1016/j.mam.2013.06.004
Schulenburg, A., Blatt, K., Cerny-Reiterer, S., Sadovnik, I., Herrmann, H., Marian, B., Grunt, T. W., Zielinski, C. C., & Valent, P. (2015). Cancer stem cells in basic science and in translational oncology: can we translate into clinical application?. Journal of hematology & oncology, 8, 16. https://doi.org/10.1186/s13045-015-0113-9
Simons, L. E., & Basch, M. C. (2016). State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain management, 6(1), 49–61. https://doi.org/10.2217/pmt.15.59
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: a neural systems approach. Neuroscience and biobehavioral reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Stuckey, D. W., & Shah, K. (2014). Stem cell-based therapies for cancer treatment: separating hope from hype. Nature reviews. Cancer, 14(10), 683–691. https://doi.org/10.1038/nrc3798
Su, Y. S., Ali, R., Feroze, A. H., Li, G., Lawton, M. T., & Choudhri, O. (2016). Endovascular therapies for malignant gliomas: Challenges and the future. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 26, 26–32. https://doi.org/10.1016/j.jocn.2015.10.019
Understanding the HIV Epidemic. (2017). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/data
Wang, S. X., Ho, E. L., Grill, M., Lee, E., Peterson, J., Robertson, K., Fuchs, D., Sinclair, E., Price, R. W., & Spudich, S. (2014). Peripheral neuropathy in primary HIV infection associates with systemic and central nervous system immune activation. Journal of acquired immune deficiency syndromes (1999), 66(3), 303–310. https://doi.org/10.1097/QAI.0000000000000167
White, H. & Venkatesh, B. (2016). Traumatic brain injury. Oxford Textbook of Neurocritical Care, 17. https://books.google.com/books?hl=en&lr=&id=o7hlCwAAQBAJ&oi=fnd&pg=PA210&dq=traumatic+brain+injury&ots=53PDiF2Jhx&sig=TPqEUTtTpGBJdRxBbZPcgO1pqpc#v=onepage&q=traumatic%20brain%20injury&f=false
What to Read Next
Also In Injury
Trending
Popular articles on BrainFacts.org