The Neurological Impacts of HIV
- Reviewed21 Aug 2023
- Author Gail Zyla
- Source BrainFacts/SfN

The first verified case of the human immunodeficiency virus (HIV), the virus that causes acquired immune deficiency syndrome (AIDS), was found in a person’s blood sample taken in 1959. The virus spread across the globe, which led to a public health epidemic in the 1980s — and by 1999, it was the fourth largest cause of death in the world. Since then, new medications have been developed to help prevent the initial contraction of HIV, lower the risk of transmission, and reduce some of the neurological complications associated with the virus.
*Currently, an estimated 39 million people worldwide live with HIV. The majority live in eastern and southern Africa, and an estimated 14% of people living with HIV are unaware that they are infected with the virus. From 2010 to 2022, the estimated number of new HIV diagnoses around the world fell by 38% from 2.2 million to 1.3 million, possibly due to targeted prevention efforts. Globally, the number of people receiving treatment for HIV has increased dramatically in recent years, particularly in developing countries. In 2022, 29.8 million people living with HIV (76% of those worldwide with HIV) were receiving life-prolonging antiretroviral therapy (ART). In 2010, only 7.7 million people were receiving this treatment.
HIV is transmitted through bodily fluids such as blood, semen, vaginal fluids, anal fluids, and breast milk. The virus attacks the immune system, specifically T cells — a type of white blood cell that helps protect the body from infection. Over time, it can destroy so many T cells that the body can’t fight off infections and diseases, eventually leading to the most severe form of an HIV infection: AIDS.
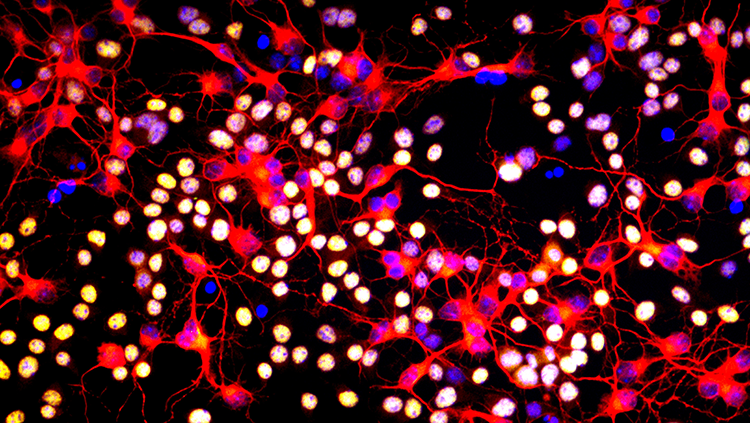
Although HIV targets the immune system, the nervous system can also be affected. HIV does not directly invade neurons, but it puts their function at risk by infecting resident immune cells in the brain like microglia. HIV also triggers inflammation that can damage the brain and spinal cord. Around half of people with HIV also develop HIV-associated neurocognitive disorders (HAND). HAND symptoms range from mild difficulty with concentration, memory, coordination, and complex decision-making to progressive dementia, called HIV-associated dementia. Even people who receive antiretroviral treatments can develop mild symptoms of HAND; however, the treatment may help prevent or even reverse mild to severe HAND symptoms in many people.
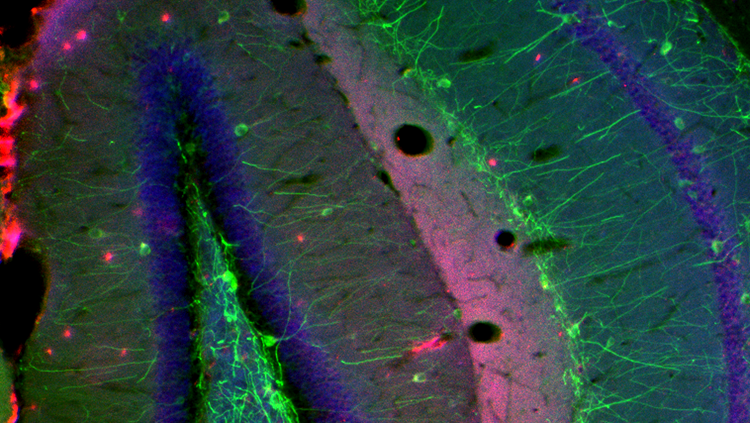
Mild forms of HAND have been reported in people with HIV infection who have no other symptoms. In advanced disease, people can develop increasing problems with concentration and memory as well as an overall slowing of mental processes. At the same time, they might experience arm or leg weakness and loss of balance, coordination, and dexterity. MRI and CT scans show brain shrinkage in people with HAND. Examination of the brains of people who die with AIDS sometimes reveals loss of nerve cells, white matter abnormalities, and damage to cellular structures involved in cell-to-cell communication. Inflammation and blood vessel disease can also be present.
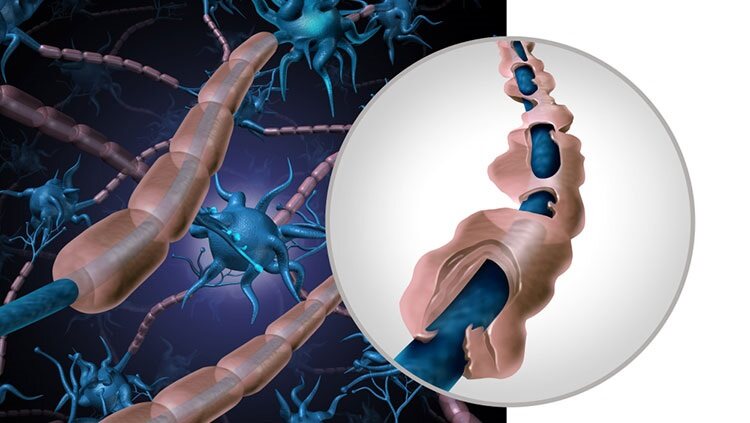
Another neurological problem common in people with HIV is peripheral neuropathy. Peripheral neuropathy involves injury to the nerves of the extremities and causes discomfort ranging from tingling and burning to severe pain. Inflammation from HIV can trigger the injury, and certain ARTs can cause the neuropathies or make them more frequent and severe. About a third of people with advanced AIDS have neuropathy.
Despite remarkable advances in new therapies, AIDS cannot be cured, and some of its neurological problems do not respond to treatment. Fortunately, combination ARTs, using three or more drugs to treat HIV and stop the virus from multiplying, can reduce the incidence of HIV transmission and severe HAND symptoms. These treatments can also improve cognitive performance and brain connectivity compared to those who have HIV and aren’t on ART. And importantly, pre-exposure prophylaxis (PrEP) medications have provided a means for prevention against initial contraction of HIV for those at-risk of contact with the virus.
*This paragraph was updated August 21, 2023 with the latest UNAIDS figures for HIV incidence, prevalence, and treatment.
Adapted from the 8th edition of Brain Facts by Gail Zyla.
CONTENT PROVIDED BY
BrainFacts/SfN
References
AIDS and HIV, Neurological Complications of. (2023). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/aids-and-hiv-neurological-complications
Bang, O. Y., Kim, E. H., Cha, J. M., & Moon, G. J. (2016). Adult Stem Cell Therapy for Stroke: Challenges and Progress. Journal of stroke, 18(3), 256–266. https://doi.org/10.5853/jos.2016.01263
Centers for Disease Control and Prevention. (2017). HIV in the United States and Dependent Areas. https://www.cdc.gov/hiv/statistics/overview/ataglance.html
Centers for Disease Control and Prevention. (2017). Stroke Facts. https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2017). Traumatic Brain Injury & Concussion. https://www.cdc.gov/TraumaticBrainInjury/
Chapman, S. N., Mehndiratta, P., Johansen, M. C., McMurry, T. L., Johnston, K. C., & Southerland, A. M. (2014). Current perspectives on the use of intravenous recombinant tissue plasminogen activator (tPA) for treatment of acute ischemic stroke. Vascular health and risk management, 10, 75–87. https://doi.org/10.2147/VHRM.S39213
Correale, J., Gaitán, M. I., Ysrraelit, M. C., & Fiol, M. P. (2017). Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain : a journal of neurology, 140(3), 527–546. https://doi.org/10.1093/brain/aww258
Doulames, V. M., & Plant, G. W. (2016). Induced Pluripotent Stem Cell Therapies for Cervical Spinal Cord Injury. International journal of molecular sciences, 17(4), 530. https://doi.org/10.3390/ijms17040530
Gereau, R. W., 4th, Sluka, K. A., Maixner, W., Savage, S. R., Price, T. J., Murinson, B. B., Sullivan, M. D., & Fillingim, R. B. (2014). A pain research agenda for the 21st century. The journal of pain, 15(12), 1203–1214. https://doi.org/10.1016/j.jpain.2014.09.004
Global HIV & AIDS Statistics — Fact Sheet. (2022). UNAIDS. https://www.unaids.org/en/resources/fact-sheet
HIV and AIDS Dementia. (2023). WebMD. https://www.webmd.com/hiv-aids/dementia-hiv-infection
Frysh, P. (2022). HIV Neuropathy: Symptoms, Causes, and Treatment. WebMD. https://www.webmd.com/hiv-aids/hiv-neuropathy-symptoms-causes-treatment
Krieger S. C. (2016). New Approaches to the Diagnosis, Clinical Course, and Goals of Therapy in Multiple Sclerosis and Related Disorders. Continuum (Minneapolis, Minn.), 22(3), 723–729. https://doi.org/10.1212/CON.0000000000000324
Martucci, K. T., Ng, P., & Mackey, S. (2014). Neuroimaging chronic pain: what have we learned and where are we going?. Future neurology, 9(6), 615–626. https://doi.org/10.2217/FNL.14.57
Matinella, A., Lanzafame, M., Bonometti, M. A., Gajofatto, A., Concia, E., Vento, S., Monaco, S., & Ferrari, S. (2015). Neurological complications of HIV infection in pre-HAART and HAART era: a retrospective study. Journal of neurology, 262(5), 1317–1327. https://doi.org/10.1007/s00415-015-7713-8
National Cancer Institute. (2017). Cancer Stat Facts: Brain and Other Nervous System Cancer. NIH. https://seer.cancer.gov/statfacts/html/brain.html
National Spinal Cord Injury Statistical Center. (2017). University of Alabama at Birmingham. https://www.nscisc.uab.edu/
Okura, H., Smith, C. A., & Rutka, J. T. (2014). Gene therapy for malignant glioma. Molecular and cellular therapies, 2, 21. https://doi.org/10.1186/2052-8426-2-21
Origin of HIV and AIDS. (2022). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/context/origin-hiv-and-aids
Pre-Exposure Prophylaxis (PrEP). (2022). Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/risk/prep/index.html
Reardon, D. A., Freeman, G., Wu, C., Chiocca, E. A., Wucherpfennig, K. W., Wen, P. Y., Fritsch, E. F., Curry, W. T., Jr, Sampson, J. H., & Dranoff, G. (2014). Immunotherapy advances for glioblastoma. Neuro-oncology, 16(11), 1441–1458. https://doi.org/10.1093/neuonc/nou212
Rosado, I. R., Lavor, M. S., Alves, E. G., Fukushima, F. B., Oliveira, K. M., Silva, C. M., Caldeira, F. M., Costa, P. M., & Melo, E. G. (2014). Effects of methylprednisolone, dantrolene, and their combination on experimental spinal cord injury. International journal of clinical and experimental pathology, 7(8), 4617–4626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152024/
Schonberg, D. L., Lubelski, D., Miller, T. E., & Rich, J. N. (2014). Brain tumor stem cells: Molecular characteristics and their impact on therapy. Molecular aspects of medicine, 39, 82–101. https://doi.org/10.1016/j.mam.2013.06.004
Schulenburg, A., Blatt, K., Cerny-Reiterer, S., Sadovnik, I., Herrmann, H., Marian, B., Grunt, T. W., Zielinski, C. C., & Valent, P. (2015). Cancer stem cells in basic science and in translational oncology: can we translate into clinical application?. Journal of hematology & oncology, 8, 16. https://doi.org/10.1186/s13045-015-0113-9
Simons, L. E., & Basch, M. C. (2016). State of the art in biobehavioral approaches to the management of chronic pain in childhood. Pain management, 6(1), 49–61. https://doi.org/10.2217/pmt.15.59
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: a neural systems approach. Neuroscience and biobehavioral reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Stuckey, D. W., & Shah, K. (2014). Stem cell-based therapies for cancer treatment: separating hope from hype. Nature reviews. Cancer, 14(10), 683–691. https://doi.org/10.1038/nrc3798
Su, Y. S., Ali, R., Feroze, A. H., Li, G., Lawton, M. T., & Choudhri, O. (2016). Endovascular therapies for malignant gliomas: Challenges and the future. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 26, 26–32. https://doi.org/10.1016/j.jocn.2015.10.019
Understanding the HIV Epidemic. (2017). Be in the KNOW. https://www.beintheknow.org/understanding-hiv-epidemic/data
Wang, S. X., Ho, E. L., Grill, M., Lee, E., Peterson, J., Robertson, K., Fuchs, D., Sinclair, E., Price, R. W., & Spudich, S. (2014). Peripheral neuropathy in primary HIV infection associates with systemic and central nervous system immune activation. Journal of acquired immune deficiency syndromes (1999), 66(3), 303–310. https://doi.org/10.1097/QAI.0000000000000167
White, H. & Venkatesh, B. (2016). Traumatic brain injury. Oxford Textbook of Neurocritical Care, 17. https://books.google.com/books?hl=en&lr=&id=o7hlCwAAQBAJ&oi=fnd&pg=PA210&dq=traumatic+brain+injury&ots=53PDiF2Jhx&sig=TPqEUTtTpGBJdRxBbZPcgO1pqpc#v=onepage&q=traumatic%20brain%20injury&f=false
Zenebe, Y., Necho, M., Yimam, W., & Akele, B. (2022). Worldwide Occurrence of HIV-Associated Neurocognitive Disorders and Its Associated Factors: A Systematic Review and Meta-Analysis. Frontiers in psychiatry, 13, 814362. https://doi.org/10.3389/fpsyt.2022.814362
What to Read Next
Also In Immune System Disorders
Trending
Popular articles on BrainFacts.org