Dating back to prehistoric times, humans have consumed opioids by extracting opium (also known as morphine) from the juice of poppy flowers.
The drug heroin is an opioid that is made (illegally) by drying morphine, adding various chemicals, and then heating it until it evaporates and becomes a powder. When injected into a vein, heroin reaches the brain in 15 to 20 seconds. Once there, it is quickly converted back to morphine, which binds to opioid receptors, switching on the brain’s reward system and flooding synapses with pleasure-inducing dopamine. The result is a brief rush of intense euphoria, followed by a few hours in a state of relaxed contentment. Opioids’ effects vary in strength, toxicity, safety, and how quickly they act.
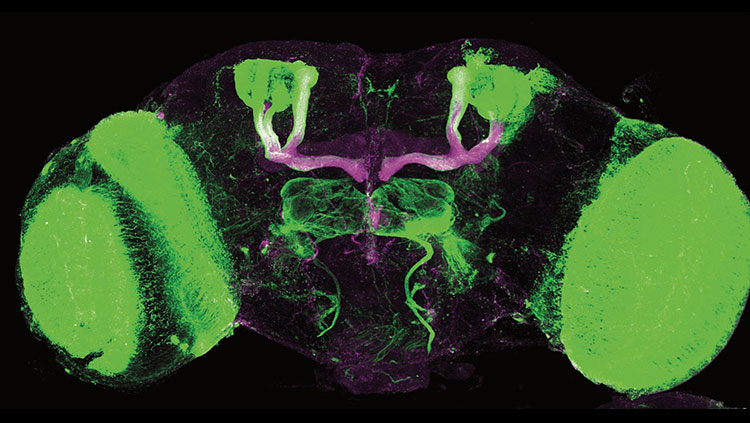
So why do our brains have opioid receptors? Our pituitary gland produces natural versions of opioids called endorphins, which help control motivation, emotion, food intake, and pain response. Laboratories produce synthetic opioids, which include heroin as well as prescription pain medicines like codeine, oxycodone (oxycontin), and fentanyl. Much more powerful than other opioids, fentanyl is used by doctors to treat severe pain. However, illegally made and distributed versions are sold on the black market and can be extremely dangerous. Opioids have many medically important uses — suppressing a cough, stopping diarrhea, and relieving pain — but, in excess, they can cause breathing to stop, the usual cause of death in an overdose.
Over the past two decades, the number of overdose deaths involving opioids (both prescription opioids and heroin) has quadrupled. Nearly 100 Americans, from every walk of life, die from opioid overdoses each day. This opioid-addiction epidemic appears to stem directly from increased use of legally prescribed opioid medications that began in the mid-1980s to treat chronic pain. In fact, about 80 percent of current heroin users say their opioid use began with prescription pain medications; once hooked, they found heroin to be cheaper and easier to get than the prescription medications. However, street heroin can be mixed with other dangerous substances, including high concentrations of fentanyl that can be immediately fatal. Another contributor to this epidemic was the 1995 introduction of a long-lasting version of oxycontin. Researchers now believe that, in medical as well as nonmedical users, addiction rather than abuse is the main driver of the opioid-overdose epidemic.
Treatment
The most effective treatment for opioid overdose is an antidote-like approach using synthetic drugs that block opioid receptors. The “antidote,” naloxone, binds to opioid receptors — without producing a biological effect — and prevents an opioid from binding. If given quickly enough, it can actually reverse a potential overdose caused by heroin or prescribed painkillers. Naloxone can be used as prevention, to limit cravings in people highly motivated to quit. Doctors sometimes prescribe naloxone to a family member of someone at risk of opioid overdose so they can administer it, and many first responders across the country are taught how to administer naloxone in cases of overdose emergencies.
The FDA has approved three medications to treat opioid use disorder: naltrexone, methadone, and buprenorphine. Naltrexone, like naloxone, blocks opioids from binding to their receptors; however, it is not an emergency drug and is generally prescribed as part of a treatment plan for opioid or alcohol substance use. Other FDA-approved drugs, methadone and buprenorphine, stimulate opioid receptors, but produce a limited high. They also reduce withdrawal symptoms from other opioids; both drugs have milder withdrawal symptoms of their own. Of the two, buprenorphine is considered to have a weaker effect than methadone, and it can be prescribed in an office setting. Suboxone, a combination of buprenorphine and naloxone, is also used to help treat opioid addiction. Researchers have found that these therapies can help deter a person from seeking heroin or other abused opioids.
Drug-based treatment for overdoses can save lives, but other strategies are also needed to treat opioid addiction itself and prevent future crises of these highly addictive substances. Psychosocial approaches, including cognitive behavioral therapy and behavioral change focused on positive reinforcement, can also be combined with drug treatments to treat opioid addiction.
Adapted from the 8th edition of Brain Facts by Alison Davis.
CONTENT PROVIDED BY
BrainFacts/SfN
References
American Lung Association. (2017). What's In a Cigarette? http://www.lung.org/stop-smoking/smoking-facts/whats-in-a-cigarette.html
Baumann, M. H., Solis, E., Jr, Watterson, L. R., Marusich, J. A., Fantegrossi, W. E., & Wiley, J. L. (2014). Baths salts, spice, and related designer drugs: the science behind the headlines. The Journal of Neuroscience. 34(46), 15150–15158. https://doi.org/10.1523/JNEUROSCI.3223-14.2014
Centers for Disease Control and Prevention & National Center for Injury Prevention and Control. (2017). Understanding Drug Overdoses and Deaths. https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html
Garnier-Dykstra, L. M., Caldeira, K. M., Vincent, K. B., O'Grady, K. E., & Arria, A. M. (2012). Nonmedical use of prescription stimulants during college: four-year trends in exposure opportunity, use, motives, and sources. Journal of American College Health. 60(3), 226–234. https://doi.org/10.1080/07448481.2011.589876
National Institute on Drug Abuse. (2015). The science behind designer drugs. https://archives.drugabuse.gov/news-events/latest-science/science-behind-designer-drugs
National Institute on Drug Abuse. (2017). Cannabis (Marijuana) DrugFacts. https://www.drugabuse.gov/publications/drugfacts/marijuana
National Institute on Drug Abuse. (2017). Cannabis (Marijuana) Research Report: Is marijuana safe and effective as medicine? https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine
National Institute on Drug Abuse. (2017). Commonly Used Drugs Charts. https://www.drugabuse.gov/drugs-abuse/commonly-abused-drugs-charts
National Institute on Drug Abuse. (2017). Drugs, Brains, and Behavior: The Science of Addiction.
Drugs and the Brain. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain
National Institute on Drug Abuse. (2017). Heroin DrugFacts. https://www.drugabuse.gov/publications/drugfacts/heroin
National Institute on Drug Abuse. (2017). Methamphetamine DrugFacts. https://www.drugabuse.gov/publications/drugfacts/methamphetamine
National Institute on Drug Abuse. (2018, July 2). The Science of Drug Use and Addiction: The Basics. https://archives.drugabuse.gov/publications/media-guide/science-drug-use-addiction-basics
National Institute on Drug Abuse. (2022). Tobacco, Nicotine, and E-Cigarettes Research Report
What are treatments for tobacco dependence? https://nida.nih.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/what-are-treatments-tobacco-dependence
National Institute on Alcohol Abuse and Alcoholism. (2017). Alcohol Facts and Statistics. https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-topics/alcohol-facts-and-statistics
What to Read Next
Also In Addiction
Trending
Popular articles on BrainFacts.org