Studies Examine Spread and Clearance of Misfolded Proteins in Parkinson’s
- Published19 Dec 2024
- Author Ailie McWhinnie
- Source BrainFacts/SfN
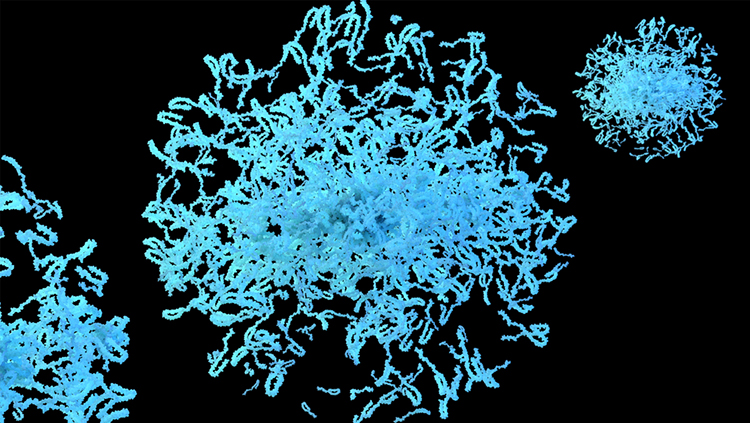
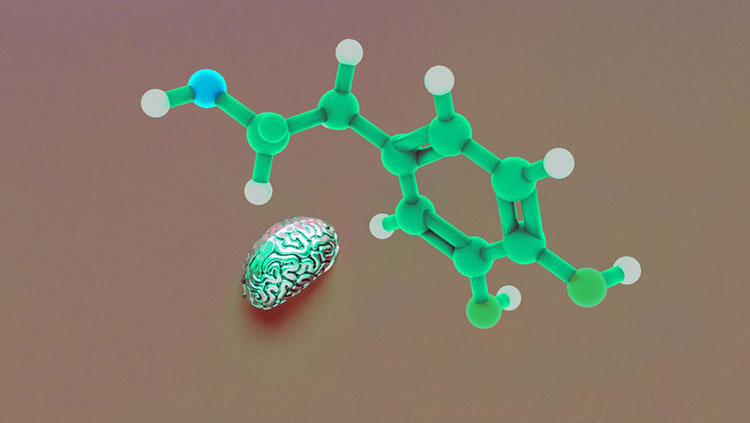
An important job for all cells is to clear out waste and toxic material — but sometimes they don’t. The buildup of such material, namely misfolded alpha-synuclein proteins, is thought to be a major driver of neurodegeneration in Parkinson’s disease.
“Alpha-synuclein is a normal protein. We all have it in our brains,” said Gus Davis, a researcher and neurologist at Washington University School of Medicine in St. Louis. “But in Parkinson’s disease, it tends to clump or aggregate.” These clumps, unlike the normal proteins, are toxic and can escape neurons to spread through the brain and into other neurons.
At the Society for Neuroscience’s annual meeting in October, researchers presented preliminary insights into the brain’s protective mechanisms against toxic alpha-synuclein and how it might fail in Parkinson’s disease.
A Crumbling Line of Defense Against Alpha-Synuclein
Neurons are not alone in the brain. Microglia, a type of immune cell, are responsible for supporting neurons and clearing harmful substances including alpha-synuclein clumps. They work by pulling in and breaking down these materials in acidic compartments called lysosomes.
“We think this may even serve as a protective mechanism,” Davis said. By disposing of clumps, microglia reduce the amount of alpha-synuclein available to infect neighboring neurons. In Parkinson’s, though, alpha-synuclein accumulates and spreads with time, leading his team to question whether the process could be failing in people with Parkinson’s disease.
Davis’ team identified a number of genes affecting the clean-up process by growing millions of microglia in a dish but rendering one gene in each cell non-functional with the gene-editing technique called a CRIPSR library.
Most of the edited microglia continued to internalize alpha-synuclein as normal, but some showed dramatic impairment or improvement, indicating their edited genes must be involved in the uptake process.
Some of those genes had been previously identified in humans as genetic risk factors for Parkinson’s disease, but why they posed a risk was unknown. Linking the initial findings to this human data supports the theory that the brain has a line of defense against alpha-synuclein, but in some people, it is weakened, increasing the chance of disease.
Other genes they identified had not been associated with Parkinson’s, so they present new targets for further studies. “We’re encouraged that this may give us a system to take results from a large unbiased screen and then combine it with patient data from human genetics,” Davis said.
Transparent Brains Reveal Patterns in Disease
Understanding the spread of alpha-synuclein through the brain has been challenging. “It is thought [alpha-synuclein] behaves somewhat like a prion,” said Yasir Gallero-Salas, a senior scientist at Gubra, a biotech company based in Denmark. The disease, or toxic aggregation of the protein, starts somewhere in the body or brain and then spreads across the nervous system, driving the degeneration of dopamine neurons.
Why dopamine neurons specifically face degeneration is a prominent question in Parkinson’s research. Technical limitations mean studies typically focus on one brain area or aspect of disease, so how these factors interact with each other can be difficult to pin down.
New methods are emerging, though, providing scientists with tools to overcome these challenges. To look at how alpha-synuclein spreads through the whole brain and how it relates to dopamine degeneration, scientists at Gubra developed a method for 3D imaging of the entire mouse brain — by making the brains transparent.
The team injected aggregated alpha-synuclein into the striatum of mouse brains, an area associated with Parkinson’s disease, and tracked its spread over the following six months.
Looking through the whole intact brain would usually be impossible because light cannot pass all the way through, so the team made the brains transparent. This is possible through a procedure called tissue clearing which removes or alters certain tissue components — like the fatty molecules around cells — to allow light to pass through more easily.
After four weeks, they started to see alpha-synuclein spread. But rather than spreading sequentially through areas closest to the injection site, alpha-synuclein first appeared in regions that were not necessarily spatially close but had the strongest neuronal connections to the injection site. These areas were the motor cortex and substantia nigra, involved in movement, and the amygdala, involved in emotion.
Studying the transparent brains more closely, Gallero-Salas’ team found that as alpha-synuclein built up throughout the brain, dopamine neurons decreased their connections with important motor areas and declined in numbers.
These findings support the theory that alpha-synuclein spreads through neuronal connections rather than to nearby neurons. Beyond this study, though, the goal of developing this method is to improve early-stage drug development. “We hope to use this platform to test different drugs to produce unbiased and accurate assessment of drug efficacies that either stop the spread of alpha-synuclein or prevent the loss of dopaminergic neurons,” Gallero-Salas said.
Like other neurodegenerative disease, Parkinson’s has proved difficult to target. But as research tools and means to match the results of animal studies with human data advance through the work of people like Davis and Gallero-Salas, researchers remain optimistic.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Calabresi, P. et al. Alpha-synuclein in Parkinson’s disease and other synucleinopathies: from overt neurodegeneration back to early synaptic dysfunction. Nature Cell Death Dis 14, 176 (2023). https://doi.org/10.1038/s41419-023-05672-9
Chen, Y. et al. APOE3ch alters microglial response and suppresses Aβ-induced tau seeding and spread. Cell 187, 2 (2024). https://doi.org/10.1016/j.cell.2023.11.029
Hansen, H.H. et al. (2020) Whole-brain three-dimensional imaging for quantification of drug targets and treatment effects in mouse models of neurodegenerative diseases. Neural Regen Res 15(12):2255-2257 (2020) https://doi.org/10.4103/1673-5374.284983
Richardson, D.S. et al. Tissue clearing. Nat Rev Methods Primers 1, 84 (2021). https://doi.org/10.1038/s43586-021-00080-9
What to Read Next
Also In Genes & Molecules
Trending
Popular articles on BrainFacts.org