Studying Genes Behind Hearing Loss Points to Treatment
- Published17 Mar 2022
- Author Alexis Wnuk
- Source BrainFacts/SfN
Karen Steel’s career in science didn’t go the way she thought it would. She studied genetics and zoology at university and then lined up a PhD to study the genetics of early development in the mouse with Professor M.S. Deol at University College London. But when she arrived at his lab, he had changed his mind. His lab had acquired mice with genetic mutations that made them deaf, and she was to study them instead. So Steel, now a King’s College London professor, pivoted. “I thought, ‘well, I’m here now. I’ll have a look into it.’”
The more she learned about the mutant mice, the more her interest in the genetics of deafness grew. “It seemed that if there was a mutation in a gene, then one day it will be possible to figure out what the mutation was and what the gene did in normal hearing,” she says. Her quest to find those genes proved successful, and in 2012, she and fellow deafness researcher Christine Petit shared the Brain Prize.
BrainFacts.org spoke with Steel about how studying the genes behind deafness can help scientists get to the bottom of all kinds of hearing impairments and point them in the direction of treatment.
What causes hearing loss?
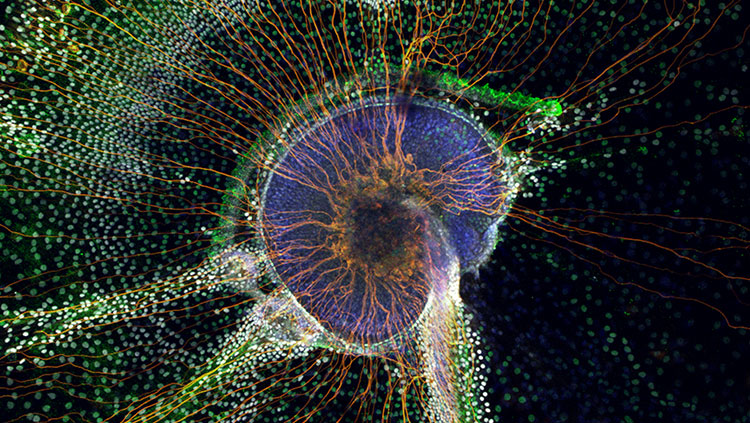
Housed within the ear are several delicate structures involved in hearing. The outer ear — the part of the ear you can see — funnels sound waves down the ear canal to the eardrum. When the eardrum vibrates, it jiggles tiny bones in the middle ear. The motion jostles the fluid in the snail shell-shaped cochlea, displacing tiny hair-like fibers on sensory cells and triggering electrical impulses.
A problem with any of the steps in the sequence can cause hearing loss. “There’s just so many different things that can go wrong with any of these different structures,” Steel says.
Most cases of hearing loss arise from problems in the inner ear, like damage to the sound-sensing hair cells or the auditory nerve that carries electrical signals from the ears to the brain. This form is called sensorineural hearing loss, and it’s the most difficult to treat. Damage to middle and outer ear structures can prevent sound waves from reaching the inner ear, leading to conductive hearing loss. In mixed hearing loss, there are problems with both the inner and the middle or outer ears.
What role do genes play in hearing loss?
Around 1 in 500 babies are born with a hearing impairment or develop it soon after birth. Genes play a role in 50-60% of these cases, with the majority resulting from a mutation in a single gene. Among cases of genetic hearing loss, about 70% are non-syndromic, meaning they occur without other medical conditions. The other 30% of cases have a genetic syndrome — like Usher syndrome or Pendred syndrome — that causes hearing loss in addition to other issues.
In the mid-90s, Steel and her collaborators found mutations in the MYO7A gene caused hearing loss in “shaker mice” — a breed of mutant mice that are hyperactive and have balance and hearing problems. They went on to show that the genetic misprint also caused hearing loss in people with Usher syndrome and some types of non-syndromic hearing loss.
Genes also play a role in hearing loss that develops later in life. “There are lots of other genes that you can have a mutation in that leads to a person having normal hearing to start with, but then their hearing gradually deteriorates,” Steel says. This can happen “when a person is in their teens or in their twenties or even in their thirties or forties.”
Even hearing loss precipitated by noise exposure can have genetic roots. Frequent exposure to loud noises, like working in a noisy factory or blasting music through your earbuds, can damage hearing. But some people may be more vulnerable than others. “We know of a number of mutations, a number of genes, which are involved in making a person more or less susceptible to noise-induced damage,” Steel says.
Steel is also searching for genetic changes that lead to age-related hearing loss. The best place to start is the long list of mutations known to cause childhood deafness, she says. Maybe profound mutations in these genes can lead to childhood deafness, while more subtle tweaks could predispose someone to hearing loss later in life. “That’s the simplest explanation,” Steel says. “I think that that's going to be true for quite a number of cases, but it’s not going to explain everything. It may well be that there are a different set of genes that we haven’t identified yet that are critical for maintaining hearing during an entire lifespan.”
In 2019, Steel and a team of researchers in the U.K. led a large-scale genetic screen of newly-generated mouse mutants and identified 38 new genes involved in hearing loss. Eleven of these genes were associated with hearing ability in people.
Yet, despite the wealth of data showing the role of genes in hearing loss, there’s a common misconception that “childhood deafness is genetic, adult-onset hearing loss is not genetic,” Steel says. “But that’s nonsense, to be honest. It’s just not true. Everything in a human being is a combination of genetics and environment.”
What can scientists learn by studying the genes involved in hearing loss?
Overall, as many as 1,000 genes may be involved in various forms of hearing loss.
Studying genes can help scientists figure out what parts of the hearing pathway have gone awry. Because genes code for specific proteins, if you know which gene is mutated, you can figure out which protein is impacted, Steel says. “You can then work out what that protein is doing in normal hearing, and you can work out what’s going wrong to cause hearing loss.”
“Genetics is just a tool for identifying the molecules involved in the molecular basis of hearing and deafness,” Steel says. “You need a molecular target to develop a treatment.”
This is the overarching goal of her research. Most of her current research focuses on the genes behind age-related hearing loss, which she predicts are “going to be a lot more complicated” than the genetic mutations underlying childhood deafness. Yet, she’s not deterred. For one thing, most people who lose their hearing in their twilight years start with normal hearing. “So, to me as a scientist, it seems … if we understand the molecules involved and the molecular changes that are involved, it ought to be possible to reverse it or at least stop it getting any worse.”
What’s more, age-related hearing loss affects a staggering number of people, and the number is only expected to grow. The WHO estimates that as many as 2.5 billion people will have hearing loss by 2050. “It’s huge numbers,” Steel says. “I think it deserves more attention than it gets.”
References
Genetics of Hearing Loss. (2015, February 18). Centers for Disease Control and Prevention. https://archive.cdc.gov/#/details?q=hearing%20loss&start=0&rows=10&url=https://www.cdc.gov/healthyschools/noise/signs.htm
Nonsyndromic hearing loss. (2020). In MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/genetics/condition/nonsyndromic-hearing-loss/
Steel, K. P. (2014). What’s the Use of Genetics? In A. N. Popper & R. R. Fay (Eds.), Perspectives on Auditory Research (pp. 569–584). Springer. https://doi.org/10.1007/978-1-4614-9102-6_30
Van Camp, G., & Smith, R. (n.d.). Hereditary Hearing Loss Homepage. Retrieved October 22, 2021, from https://hereditaryhearingloss.org/
What is Hearing Loss in Children? (2019, March 21). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/hearingloss/facts.html
World Report on Hearing. (2021). World Health Organization. https://www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/highlighting-priorities-for-ear-and-hearing-care
BrainFacts.org welcomes all your brain-related questions.
Every month, we choose one reader question and get an answer from a top neuroscientist. Always been curious about something?







