Glia: Earning Some Respect
- Published9 Jul 2014
- Reviewed9 Jul 2014
- Source The Dana Foundation
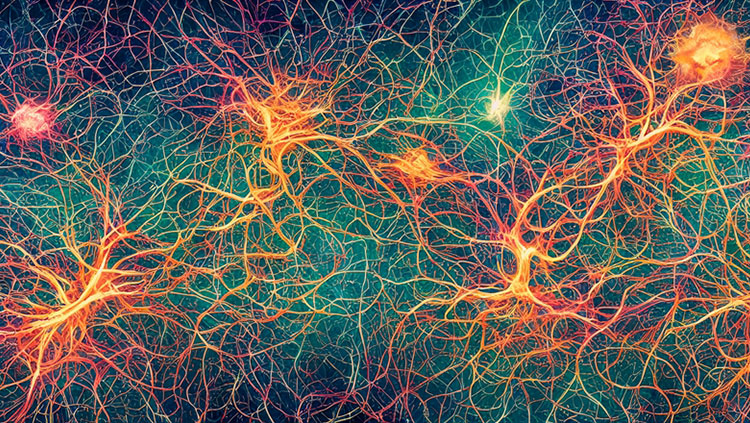
Glial cells may no longer be dismissed as "brain glue," but the idea persists that these, the most numerous cells in the brain, are essentially handmaidens to neurons that become worthy of attention only when they get mixed up in bad things like inflammation.
"If you look at a neuroscience text, there's maybe half a chapter about glia," says Donna M. Wilcock, of the Sanders-Brown Institute on Aging at University of Kentucky. "If you're not in the field, the view is that they're bystanders: They sit around the synapse, do a bit of regulation of glutamate, maybe help with the blood brain barrier, but beyond that do very little."
That view seems to be changing, as evidence accumulates that glia-the star-shaped cells called astrocytes, in particular-play a vital role in brain function, which when disrupted can have severe consequences. Stephen J. Crocker, director of the glial pathology lab at University of Connecticut, says that he and others now use the term "gliopathies" to describe conditions where astrocytes appear to have a causative role in disease, such as amyotrophic lateral sclerosis (ALS). "[Those] where subtle changes could be detrimental to the neuron we call 'gliodystrophies,'" he said.
"The fact that there are names for it suggests these ways of thinking are no longer in back alleys of science, but becoming an established paradigm."
A vital balance
Recent studies at UCLA, reported online in Nature Neuroscience in March 2014, suggest glial involvement in Huntington's disease. The research linked changes in astrocytes to the dysfunction of medium spiny neurons (MSNs) in the striatum, which is characteristic of HD.
Earlier research had found aggregates of mutant huntingtin (mHTT), the hallmark protein of HD, in astrocytes of a mouse model of the disease and in post-mortem tissue of people who had died of HD. "This raised the possibility that it could be a contributory factor," says study co-author Baljit S. Khakh, professor of physiology and neuroscience at the university. But how was unclear.
His study highlighted a well-known function of astrocytes: regulating extracellular potassium. In two mouse models of HD, the researchers found that mHTT-containing astrocytes had reduced Kir4.1 channels, which astrocytes use to pull potassium out of surrounding fluid to maintain homeostasis. As the flow of potassium into astrocytes fell, levels in extracellular fluid rose--enough to increase excitability of nearby MSNs. (Hyperexcitability may be a main reason for neuron death in HD).
"This suggested that disruption of potassium homeostasis could lead to downstream consequences in the neurons," Khakh said.
Restoring Kir4.1 channels by virally inserting the gene that produces the protein, the researchers found, normalized K concentration in the motor cortex, and ameliorated symptoms. "It didn't rescue everything, but you could see improvement in walking, and a strong effect on general health and survival, at least for a short time," says co-author Michael Sofroniew, professor of neurobiology at UCLA. You could pick out the animals that had viral rescue."
Although much research is needed before clinical applications can be envisioned, "conceptually, viral rescue of the potassium channel in astrocytes in humans is not farfetched," he says. "But you have to be realistic about the role of astrocytes. Fixing them alone won't fix the disease, but just fixing neurons won't, either."
More generally, Sofroniew says, this study adds to research "putting astrocyte physiology into the big picture… the interdependence of cells for normal brain function."
A lesson that Khakh draws from his findings is that even a "support" role-buffering potassium- "can be very important within the context of this circuit." Could a similar process contribute to disease elsewhere in the brain? "Colleagues working in other neurological diseases are interested in this," he says.
Donna Wilcock, for one. The UCLA findings "could point to [potassium dysfunction in astrocytes] as a common pathway that might be targeted in multiple disorders," she says.
Her own research several years ago implicated loss of homeostasis-maintaining astrocyte channels, including Kir4.1, in vascular dementia and possibly Alzheimer's as well. But whether simply supplying the proteins without a means to anchor them to the astrocyte would restore function, she thought then, was questionable.
"This research shows that the cell finds a way," Wilcock says. "The rescue operation-that's the star of the paper.... I'm very interested in pursuing something along these lines." Beyond its specifics, the UCLA research "points to the absolutely critical need for better understanding the molecular processes underlying astrocyte function."
Regrowth and repair
Astrocytes may have the potential to ease the symptoms of Parkinson's disease, according to research published online in January 2014 in EMBO Molecular Medicine. While many different types of neurons die in Parkinson's, most death is due to dopamine deficiency, so replacing or augmenting that neurotransmitter is the primary therapy. The idea of transplanting dopamine-producing neurons has tantalized researchers for years, but results have been disappointing.
Christopher Proschel and colleagues at University of Rochester took a different tack: transplanting neuroglia that could promote regeneration of neurons impacted by Parkinson's. They generated a subtype of astrocyte by incubating embryonic glial precursor cells with bone morphogenic protein, a naturally-occurring molecule that promotes tissue differentiation.
The resulting astrocytes, GDAsBMP, produced generous amounts of chemicals that promote neuron growth and survival [e.g. brain-derived neurotrophic factor (BDNF), glial-derived neurotrophic factor (GDNF) and neurturin], and antioxidant proteins that have additional neuroprotective effects.
When transplanted into a rat model of PD after symptoms had already emerged, the astrocytes essentially normalized levels of tyrosine hydroxylase, a key enzyme in dopamine production and a marker for loss of dopaminergic neurons. What was more, the treated animals recovered some motor functions that continued to decline in untreated controls.
The researchers observed that dopaminergic neurons were not the only ones rescued by GDAsBMP. "To me, the most impressive finding was the ability to recover the interneuron population," local circuit neurons, says Proschel. "You can replace dopaminergic neurons with various methods, but here we have the opportunity to address other neurons as well--a real potential to intervene."
Whether the astrocytes used in the study occur spontaneously in the human brain is uncertain, he said, but they may correspond to subtypes arising during development.
Proschel has used the same approach to regenerate neurons in other situations: in an earlier study, transplanting GDAsBMP promoted recovery in rats after spinal cord injury. "We saw a neuroprotective effect close to the injury site, and increased axonal outgrowth, and hypothesized that this might also work in a neurodegenerative model like Parkinson's," he said.
He is now investigating a role for GDAsBMP in traumatic brain injury, where "the data is encouraging and looks consistent with what we've seen in spinal cord injury. Stroke is another very interesting target area," he says.
While clinical trials remain a distant prospect, he notes that substantial quantities of GDAsBMP can be generated from very little fetal tissue, and that it may be possible to derive them from induced pluripotent stem cells (iPSCs) grown from adult tissue.
"What was impressive [in the current study]," Stephen Crocker says, "was that the researchers introduced the cells weeks after the lesion was inflicted; this resembles the clinical situation, where people come in already showing signs of the disease, not in its earliest stages. They set the bar quite high, and then were able to jump over it."
The findings, he says, strengthen earlier research implying a role for astrocyte dysfunction in Parkinson's-that the disease is, in effect, a gliodystrophy. "The tremendous success of this study, one of the first of its kind, would argue that transplanting neurons in Parkinson's could be viewed as putting wood in a fire, but astrocytes can perhaps damp down the intensity of the flame, to provide longer term, superior restoration of circuitry."
- Carl Sherman
CONTENT PROVIDED BY
The Dana Foundation is a private philanthropic organization that supports brain research through grants and educates the public about the successes and potential of brain research.
Also In Cells & Circuits
Trending
Popular articles on BrainFacts.org