Food for Thought: Obesity and Addiction
- Published20 Apr 2012
- Reviewed20 Apr 2012
- Source BrainFacts/SfN
Could candy be addictive, like cocaine or nicotine? Until recently, many believed overeating and obesity were caused by a lack of “willpower”. But new research suggests that certain diets — those high in fat and sugar — can lead to changes in the brain that are similar to those seen with drug addiction. These findings are changing our understanding of what may drive overeating.
Many people find it difficult to stop eating. Instead of having a single scoop of ice cream, they devour the entire pint. And they do so even when they are not hungry.
For many years, overeating and obesity were viewed as failures of willpower. Doctors and nutritionists advised overweight people to eat less and exercise more to shed excess pounds. But new research suggests it may not be that simple.
Scientists are finding high-fat, high-sugar foods can trigger lasting brain changes that might make it difficult to resist overeating. Furthermore, those changes resemble what happens in the brain when someone is addicted to drugs, such as nicotine, alcohol, and cocaine.
The implications of this research are considerable. More than 33 percent of adults and 17 percent of children and teenagers in the United States are obese. Some 300,000 deaths are attributed to obesity-related diseases each year, making it the nation’s second-leading cause of preventable death. In addition, the estimated annual medical cost of treating obesity-related diseases in the United States is staggering: $147 billion.
By studying how food alters brain structures and functions, scientists are learning more about the neurobiological factors behind the obesity epidemic. This ongoing research is enabling scientists to:
- Understand how food affects the brain’s reward system.
- Develop more effective therapies for preventing and treating obesity.
One of the central players in the regulation of appetite is the hormone leptin. Produced in the body’s fat cells, leptin lets the brain know when there is enough energy stored in those cells. It tells the brain when you can stop eating, at least for a while. Some evidence suggests the brains of obese individuals are less sensitive to the hormone. In extremely rare cases of obesity — those in which the body produces no leptin because of a genetic mutation — overeating was curtailed and weight was lost after leptin injections.
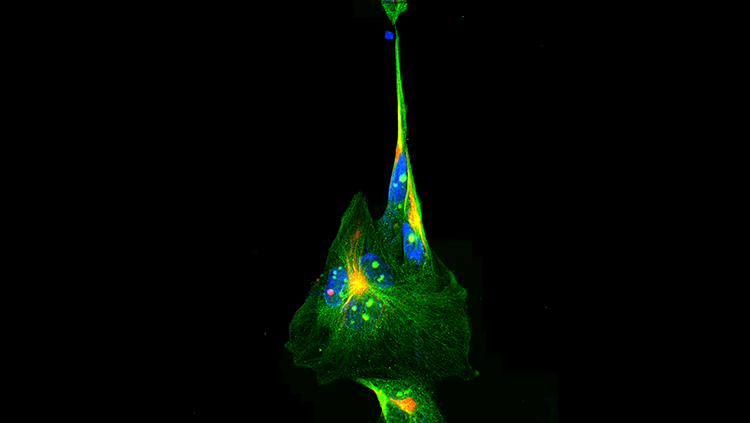
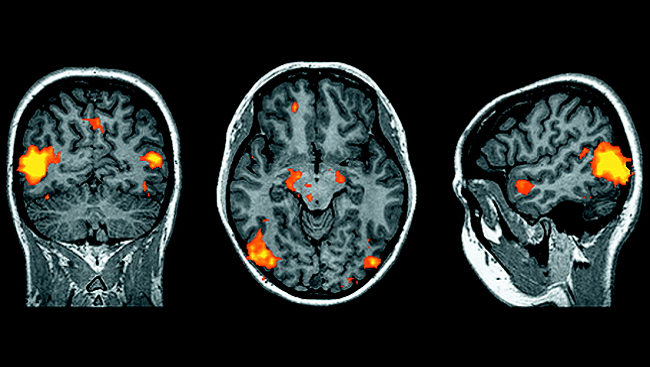
Scientists learned early on that leptin acted in the hypothalamus, a brain structure involved in the regulation and control of hunger. More recently, they discovered leptin also influences appetite by acting in a midbrain region known as the ventral tegmental area (VTA). This region contains dopamine neurons, which play a key role in the brain’s reward system — the source of the feeling of pleasure we get when we eat certain foods — and in the development of drug addictions.
Studies involving rats showed junk food diets produced addiction-like behavior as well as dopamine-related changes in the brain. In one study, rats were divided into three groups. One group was fed regular rat food. A second group was given access to fatty or sugary foods, such as sausage, bacon, cheesecake and frosting, for one hour a day. A third group was allowed to munch on the junk food whenever they wanted.
The second group quickly started binge eating the junk food, consuming most of their daily calories during the one hour they had access to the junk food. The third group not only gorged on the junk food, they also became obese. The researchers identified one possible reason why. Dopamine receptors in the reward circuitry of the obese rats had become desensitized, potentially compelling the animals to eat increasing amounts of the food to get the same level of pleasure from it. A similar effect on dopamine receptors is associated with drug addiction, and may explain why addicts crave increasing amounts of a drug.
But overeating wasn’t the only addictive-like behavior observed among the obese rats. The rats also showed compulsive-like intake of food. To test for this, all the rats were trained before the study to anticipate and try to escape a small electric shock to their feet when a light came on. But after the rats became obese, they stopped taking evasive action. When the light appeared, they kept eating. This behavior — ignoring the threat of punishment — also occurs among rats that have extended access to cocaine and is thought to reflect the development of compulsive-like consumption.
In other research, scientists discovered another similarity with drug addiction. When rats fed junk food were suddenly switched back to a healthier diet, they avoided anxiety-inducing situations — just as they do when going through withdrawal from cocaine and other addictive drugs.
Tests showed these rats had five times the normal amount of corticotropin-releasing factor (CRF) mRNA in their brains during this denial period. CRF helps regulate fear, anxiety, and stress. Once the rats were put back on a junk food diet, they no longer avoided stressful situations, and their CRF levels returned to normal. They also began to overeat even more than before — a finding that may suggest why people who go on and off diets tend to find it increasingly difficult to lose weight.
Through other intriguing research, scientists discovered that a junk food diet can alter the production of dopamine and other genes in the brain’s reward system — even after the diet is abandoned for a healthier one. Studies also found these brain changes can be passed on from pregnant mice to their offspring, making the mice pups more vulnerable to both obesity and addictive-like behaviors in adulthood. Such findings may help explain why overcoming obesity is much more complicated than “saying no” to junk food and may point to possible interventions to help people struggling to make positive behavioral change.
CONTENT PROVIDED BY
BrainFacts/SfN
Also In Archives
Trending
Popular articles on BrainFacts.org