Post-Traumatic Stress Disorder
- Published16 Mar 2009
- Reviewed23 Mar 2013
- Source BrainFacts/SfN
Natural disasters, war, violent physical attacks, serious accidents, and other traumatic events are, sadly, all too common. Most people who survive such trauma are able to feel “normal” again within a few weeks or months. But for others, the fear, anxiety, helplessness, and other intense emotions experienced during the event linger, causing a debilitating psychiatric condition known as post-traumatic stress disorder (PTSD). Why are some people more susceptible than others? Research into the underlying genetics and neurobiology of PTSD is helping to answer that question—and leading to more effective treatments.
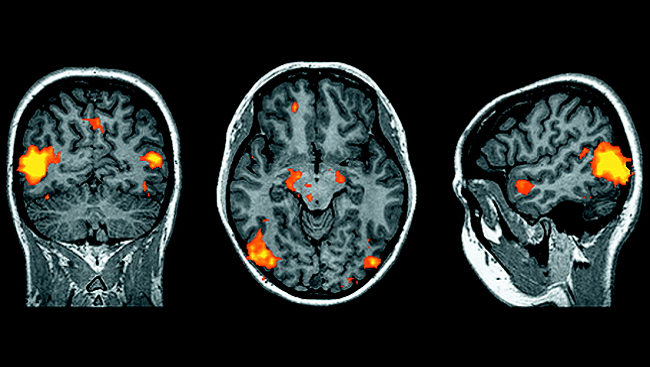
Patients with PTSD have heightened levels of norepinephrine, a chemical involved in arousal and stress. High levels of this chemical strengthens the emotional reactions of the amygdala, a brain region involved in the fear response, while weakening the rational functions of the prefrontal cortex, which normally allows us to suppress troubling memories and thoughts. Research shows that a drug called D-cycloserine, when used in combination with behavioral therapy, appears to enhance the fear extinction process.
With a new generation of U.S. soldiers coming home after prolonged exposure to combat-related stress or trauma, understanding and treating post-traumatic stress disorder (PTSD) has taken on an increased sense of urgency. According to one study, up to 14 percent of returning military personnel who served in Iraq or Afghanistan report symptoms of PTSD or major depression. But soldiers aren’t the only Americans at risk for this debilitating neuropsychiatric disorder. According to the National Institute of Mental Health, about 3.5 percent of American adults (7.7 million individuals) struggle with PTSD during any given year.
Unfortunately, current drug and behavioral treatments for PTSD are often unable to reduce or eliminate symptoms that include intrusive memories, emotional numbness, and insomnia. In recent years, however, scientists have begun to piece together some of the neurobiological puzzles behind this complex disorder, offering new hope to its sufferers. Such research is leading to:
- Greater knowledge of how psychological trauma alters brain structure and function.
- A deeper understanding of who is susceptible to PTSD.
More effective treatments for PTSD and related mental health disorders, such as depression and panic disorder.
One of the major unanswered questions about PTSD involves susceptibility. Not everybody who experiences psychological and/or physical trauma develops the disorder. Research now suggests that at least some of the risk for PTSD is genetic—perhaps as much as 40 percent, according to a multigenerational study of survivors of a devastating 1988 Armenian earthquake.
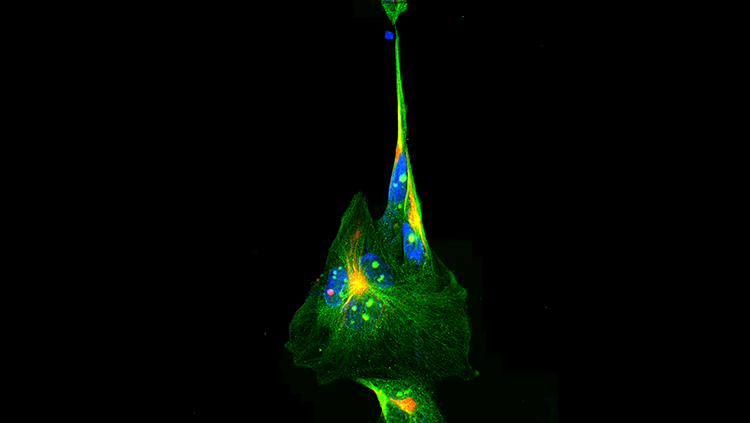
The identity of the genes involved in PTSD susceptibility remains a mystery, although one likely candidate is a gene called FKBP5. The protein produced by this gene helps stress hormones bind with their receptors on brain cells and, thus, helps regulate the brain’s response to stress. A study of adults who experienced childhood abuse found that those with certain genetic variations in this stress-related gene were significantly more likely to have PTSD symptoms than adults who were abused but lacked those variations.
Many years ago, scientists noticed that people with PTSD tended to have a smaller-than-average hippocampus, an area of the brain involved with memory. For example, some Vietnam War combat veterans with PTSD have smaller hippocampi than veterans without the symptoms. Is a change in hippocampal size brought about by stress or a preexisting risk factor? A study revealed that both Vietnam veterans with PTSD and their non-combat identical twin brothers had small hippocampi. This finding shows how hereditary factors and experience (the stress of a traumatic event) share in the development of PTSD.
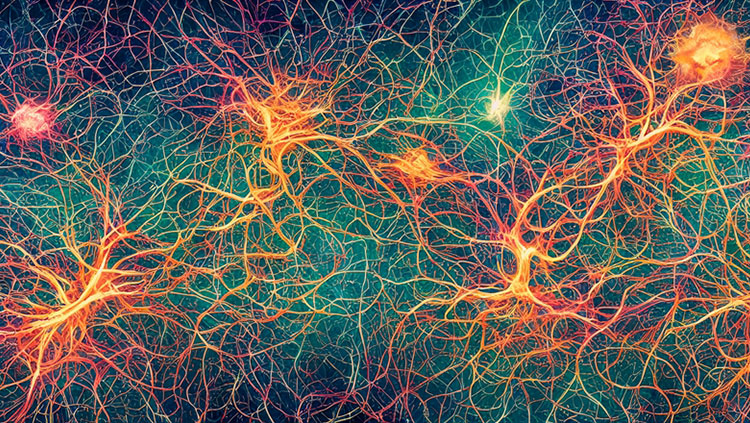
Other research has found that the amygdala, a brain region involved in the fear response, is hyper responsive in PTSD combat veterans in some conditions. This finding may explain why people with PTSD have an inability to learn to feel safe after their initial trauma. Scientists have identified specific brain circuits involved in regulation of fear and safety learning —. Drugs that target these cells might prove helpful in treating PTSD.
One such promising drug is D-cycloserine, an antibiotic that is also used experimentally to treat fear of heights. When used in combination with behavioral therapy, D-cycloserine appears to enhance the fear extinction process. Different classes of drugs targeting brain plasticity, cell excitation and other key molecular processes implicated in PTSD, are being actively studied both in animal models of this disorder and in PTSF patients
Traumatic stress cannot always be avoided. But research is pointing to new and more effective ways of helping individuals successfully prevent or break the disabling cycle of recurring PTSD symptoms.
CONTENT PROVIDED BY
BrainFacts/SfN
References
Binder EB, Bradley RG, Wei L, Epstein MP, Deveau TC, et al. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA. 1291-1305 (2008).
Goenjian AK, Noble EP, Walling DP, Goenjuian HA, Karayan IS, Ritchie T, Bailey JN. Heritabilities of symptoms of posttraumatic stress disorder, anxiety, and depression in earthquake exposed Armenian families. Psychiatric Genetics 18(6):261-266 (2008).
Yehuda R, Engel SM, Brand SR, Seckl J, Marcus SM, et al. Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. The Journal of Clinical Endocrinology and Metabolism. 90(7):4115-4118 (2005).
Yehuda R, Teicher MH, Seckl JR, Grossman RA, Morris A, Bierer LM. Parental post-traumatic stress disorder as a vulnerability factor for low cortisol trait in offspring of holocaust survivors. Archives of General Psychiatry. 64(9): 1040-1048 (2007).
Also In Archives
Trending
Popular articles on BrainFacts.org