The Neuroscience of Stress
- Published19 Jun 2018
- Reviewed19 Jun 2018
- Author Alison Caldwell
- Source BrainFacts/SfN

Anyone who has ever fretted over an exam or a looming deadline at work knows what stress feels like. As it turns out, stress can be a good thing, helping our bodies and brains stay sharp and alert, ready to react to any surprises life throws in our way. But, chronic stress can wreak havoc, triggering a host of maladies including heart disease, high blood pressure, depression, and anxiety.
Neuroscientists are beginning to reveal how chronic stress exacts such a hefty toll. In doing so, they are piecing together how parental stress affects offspring, the biochemical hallmarks of stress in children, and how specialized brain cells influence fear and anxiety responses.
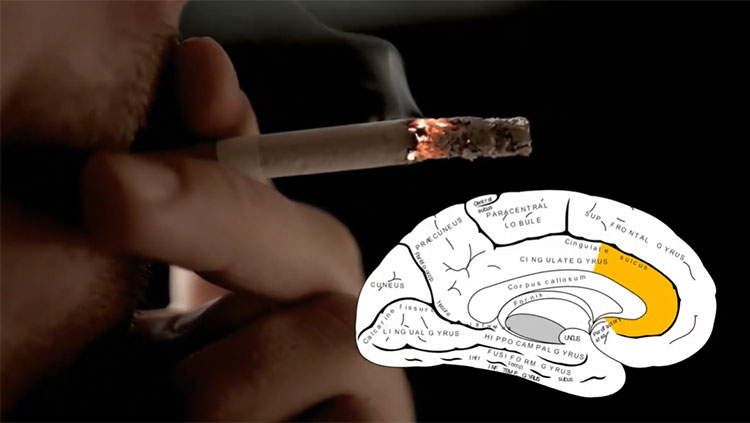
The response to short-term stress is critical for survival. It powers the “fight-or-flight” response that allows animals to respond quickly to danger signs. When we’re startled, or acutely stressed “fear center” of the brain, called the amygdala activates our central stress response system. Known as the hypothalamic-pituitary-adrenalcortical (HPA) axis because it is comprised of the hypothalamus, pituitary gland, and the adrenal cortex, this stress response system regulates hormones, particularly the stress hormone cortisol. By rapidly increasing glucose levels, speeding the heart rate, and increasing blood flow to the muscles in our arms and legs, this stress response allows us to respond to a threat. After the danger has passed, the system works to return hormone levels to normal.
When stress becomes chronic, this system is amped up all the time. The same hormones that are so important for the fight-or-flight response can lead to digestive issues, trouble sleeping, and a weakened immune system, making a person more susceptible to viruses like the flu and chronic health problems.
“Because stress changes the way the brain’s neurons communicate with each other, chronic stress can cause our brains, nervous systems, and our behavior to adjust to a vigilant and reactive state,” says Bruce McEwen, a neuroscientist from Rockefeller University.
That constant vigilance can lead to devastating mental and physical health conditions for the person experiencing it. It can also affect their offspring. It is well-established that maternal stress has deleterious effects on her offspring. But Jennifer Chan from the University of Pennsylvania wanted to know how a father’s stressful experiences would affect his offspring. So, she studied male mice that experienced mild, chronic stress. The offspring of those mice had a “blunted” hormonal stress response — an effect linked to disorders like post-traumatic stress disorder (PTSD). She found stress changed the expression of genes in sperm and altered its maturation. That may have altered the brain development of their offspring.
“If we can understand how parental experiences impact offspring health,” Chan says, “Then we may be able to identify those parental experiences as risk factors, and in the future this could lead to earlier interventions for children who may be at risk.”
Because our brains are still developing throughout childhood and early adulthood, pediatric trauma can be especially damaging. While working to find new therapies for stress disorders like PTSD, Brianna Mulligan at the University of New Mexico discovered that changes in DNA methylation, a process by which genes are turned “on” or “off,” in children who had experienced trauma. These abnormal DNA methylation signatures may help physicians identify children who are suffering from trauma. And, since DNA methylation is reversible, it may be possible to develop aid trauma recovery treatments capable of reversing the methylation.
Researchers are exploring other avenues to develop treatments for PTSD. An intriguing one involves non-neuronal brains cells called astrocytes. Long thought of as mere support cells, astrocytes also play a role in the brain’s immune response. Meghan Jones, of the University of North Carolina, found chronically stressed mice possessed elevated levels of a molecule called interleukin-1-β (IL-1) in the astrocytes of the hippocampus, a brain area critical to learning and memory.
IL-1 is known as a cytokine, a class of molecules regulating the brain’s response to illness. When Jones and her colleagues blocked the receptor for IL-1 and exposed them to chronic stress, they did not develop characteristic fear and anxiety.
Many studies offer early clues to how stress causes negative effects and potential pathways to prevent those effects. And, that is something that McEwen says should spur optimism that one day we will be able to prevent the effects of chronic stress and PTSD.
CONTENT PROVIDED BY
BrainFacts/SfN
Also In Emotions, Stress & Anxiety
Trending
Popular articles on BrainFacts.org