Macular Degeneration: Searching for a Treatment
- Published3 Sep 2014
- Reviewed3 Sep 2014
- Author Allison Curley
- Source BrainFacts/SfN
By 2020, an estimated 196 million people worldwide will be living with age-related macular degeneration — a chronic disease characterized by the progressive breakdown of the macula, the region of the retina that makes the sharp, central vision critical for such activities as reading the words off a page possible.
As the age of the world population continues to rise, scientists suspect that so too will cases of macular degeneration. According to recent projections, some 288 million people will face blindness from the disease by 2040.
While there is currently no cure for macular degeneration, scientists believe that by repairing, replacing, or working around diseased cells in the macula, future treatments will be better able to slow the course of the disease and help patients regain their sight.
Patchy Vision
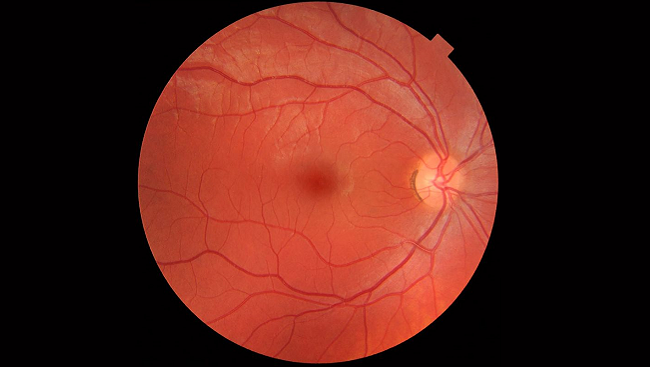
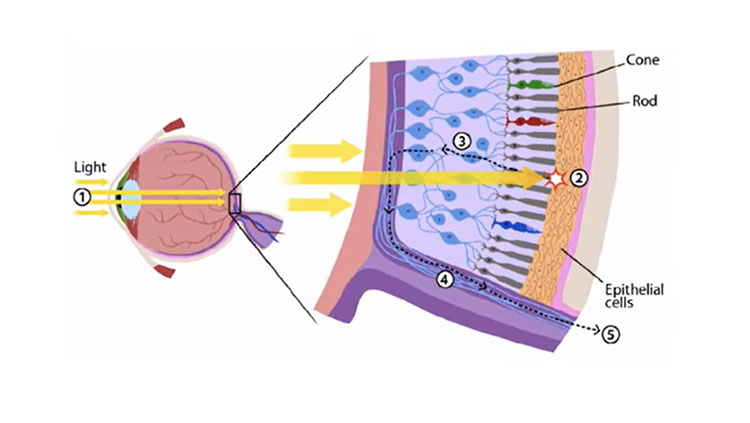
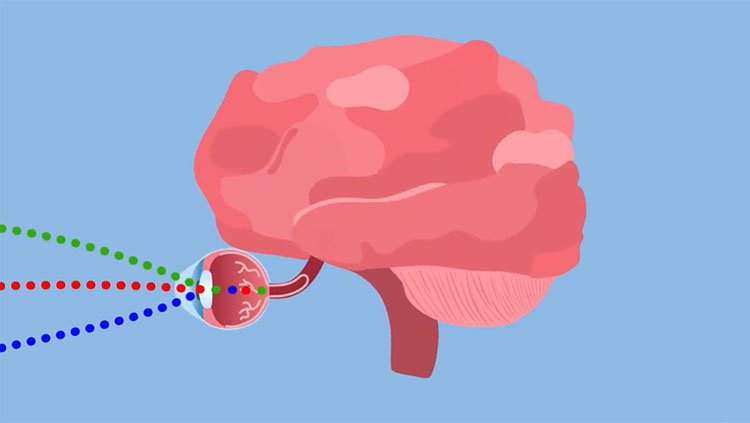
Vision begins when light enters the eye, first passing through the cornea and lens, which brings the light into sharp focus, and then onto the retina at the back of the eye. In the retina, specialized neurons called photoreceptors convert light into electrical signals that are passed to cells in other areas of the brain that interpret visual information.
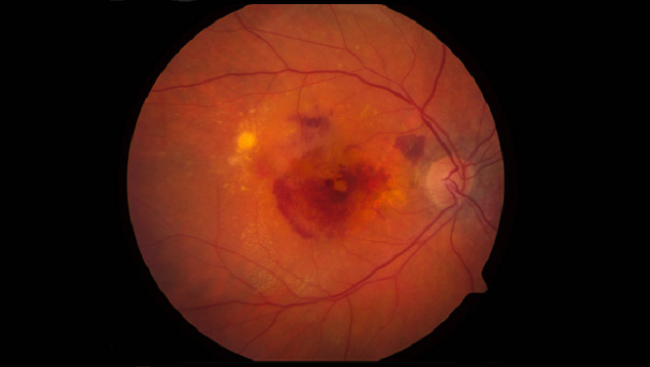
In macular degeneration, retinal pigment epithelial (RPE) cells — cells that bolster the photoreceptors in the macula — begin to break down. Without the support of these cells, photoreceptors begin dying off. In advanced stages of the disease, some patients develop large areas of degenerate RPE and photoreceptors called geographic atrophy. As Marco Zarbin, an ophthalmologist at Rutgers New Jersey Medical School describes it, this advanced type of damage to the macula occurs "much like a lawn that develops dry patches." As the disease advances, so does the size and number of the patches, resulting in a progressive deterioration of vision.
Another mechanism by which patients with late-stage macular degeneration develop severe vision loss involves the growth of abnormal blood vessels under the retina, where they leak fluid and blood, causing severe damage to photoreceptors. Although only 10 to 15 percent of all patients develop what is known as "wet" macular degeneration, if left untreated, it accounts for 80 to 90 percent of the blindness associated with the disease.
People generally fail to detect changes in vision early on in the course of macular degeneration. However, eye doctors are able to diagnose even early stages of the disease based on the accumulation of deposits called drusen in and around the macula — a tell-tale sign of the disorder. As macular degeneration progresses, visual distortions and blind spots in the central line of vision become more apparent, eventually leaving only peripheral vision intact in the most advanced stages of the disorder.
People with late-stage macular degeneration in both eyes are often able to navigate familiar environments, such as a home or office, but lose the ability to perform routine activities such as cooking or recognizing the face of a friend. These and other challenges can lead patients with macular degeneration to experience high rates of depression.
Slowing Vision Loss
As people age, particularly once they reach their 60s, their likelihood of developing macular degeneration increases. These risks increase even more for smokers and those with a family history of macular degeneration. And, while there is no cure for macular degeneration, recent studies have revealed new clues about how to slow the progression of the disease into blindness.
For instance, a large five-year clinical trial by researchers at the National Eye Institute found that people at high risk for developing late-stage macular degeneration who take a combination of high doses of vitamin C, vitamin E, beta-carotene, zinc, and copper are 19 percent less likely to develop advanced vision loss. In a follow-up study, researchers discovered that replacing beta-carotene with the antioxidants lutein and zeaxanthin may provide a safer, yet equally effective alternative for patients.
Another therapy has shown some promise for slowing vision loss in people with "wet" macular degeneration. Recent studies show that by injecting drugs into the eye that block the growth of new blood vessels under the retina, vision loss can be stabilized in 95 percent of patients for at least two years. About one-third of the people who receive this therapy also experience improved sight, enabling them to read smaller letters two lines lower on a standard eye chart.
Although these drugs are very beneficial for treating the symptoms of wet macular degeneration, the need for monthly injections and the risk of infection from the injections are significant drawbacks. As a result, scientists continue to search for new methods to deliver the drugs over longer periods of time and alternative ways to stop the blood vessels from damaging the retina.
Returning Sight to the Blind
Even as scientists look for new ways to stall vision loss in people with macular degeneration, they are focused on techniques that may one day boost vision for people living with the disorder.
Scientists have been successful in using gene therapy to return sight to people with choroideremia, a disorder that leads to total blindness by middle age, and Leber congenital amaurosis, a disease that affects infants and children. Both diseases are caused by mutations to a single gene, making patients with these disorders ideal candidates for therapies that involve replacing mutant genes with healthy ones.
According to Robert MacLaren, an ophthalmologist who studies choroideremia at Oxford University, if scientists are able to similarly narrow in on the genes contributing to macular degeneration, gene therapy could one day be used to improve outcomes for people living with the disease. However, MacLaren cautioned that identifying the genes contributing to macular degeneration will likely take time. A recent study of more than 17,000 people with macular degeneration identified seven spots in the genome that increase the risk of developing the disease.
Other scientists believe stem cells may offer a good option for bolstering the dying photoreceptors present in macular degeneration. Kang Zhang, an ophthalmologist at the University of California, San Diego, found that when he transplanted human retinal stem cells under the retina of rats that were experiencing early stages of retinal degeneration, the new cells were able to integrate into the diseased retinal tissue. As a result, rats that received the stem cell transplants were able to see better and had a greater number of photoreceptors than animals that did not receive the therapy. If replicated in humans, Zhang says this approach could someday be used to prevent vision loss in people in the early stages of macular degeneration.
Another potential treatment option for macular degeneration involves rerouting vision around the photoreceptors that are ravaged by disease via a prosthetic retina. Such a technique allows visual stimuli to essentially "jump over the damaged area," Sheila Nirenberg, a neuroscientist at Weill Medical College of Cornell University, explains.
Nirenberg's research has helped to uncover the relationship between visual stimuli and the activity of ganglion cells, which transmit visual information from the retina to the rest of the brain. With this knowledge, Nirenberg created a computerized prosthetic — a tiny camera worn in the patient's glasses — that takes in visual information and transmits the code directly to ganglion cells using optogenetics (a technique that uses light to control neurons). Nirenberg hopes to begin testing this approach of bypassing the diseased photoreceptors in people within two years.
In addition to these specific strategies to prevent vision loss or restore sight in macular degeneration, Zarbin explained that recent advances in high-resolution imaging will lead to faster diagnosis, a better understanding of how the disease progresses, and more accurate tests of potential therapeutics. With so many different lines of research underway, Zarbin says he expects to see better treatments for the late stage of the disease "within a decade."
CONTENT PROVIDED BY
BrainFacts/SfN
References
AMD Gene Consortium. Seven new loci associated with age-related macular degeneration. Nature Genetics. 45(4), 433-439e2 (2013).
Dawson SR, Mallen CD, Gouldstone MB, Yarham R, Mansell G. The prevalence of anxiety and depression in people with age-related macular degeneration: a systematic review of observational study data. BMC Ophthalmology. 14(1), 78-84 (2014).
Diniz B, Thomas P, Thomas B, Ribeiro R, Hu Y, et al. Subretinal implantation of retinal pigment epithelial cells derived from human embryonic stem cells: improved survival when implanted as a monolayer. Investigative Ophthalmology and Visual Science. 54(7), 5087-96 (2013).
Fernández-Robredo P, Sancho A, Johnen S, Recalde S, Gama N, et al. Current treatment limitations in age-related macular degeneration and future approaches based on cell therapy and tissue engineering. Journal of Ophthalmology. 510285 (2014).
Finger RP, Guymer RH, Gillies MC, Keeffe JE. The impact of anti-vascular endothelial growth factor treatment on quality of life in neovascular age-related macular degeneration. Ophthalmology. 121(6):1246-1251 (2014).
Luo J, Baranov P, Patel S, Ouyang H, Quach J, et al. Human retinal progenitor cell transplantation preserves vision. Journal of Biological Chemistry. 289(10),6362-71 (2014).
MacLaren RE, Groppe M, Barnard AR, Cottriall CL, Tolmachova T, et al. Retinal gene therapy in patients with choroideremia: initial findings from a phase 1/2 clinical trial. Lancet. 383(9923),1129-37 (2014).
Nirenberg S, Pandarinath C. Retinal prosthetic strategy with the capacity to restore normal vision. Proceedings of the National Academy of Sciences. 109(37),15012-7 (2012).
Rattner A, Nathans J. Macular degeneration: recent advances and therapeutic opportunities. Nature Reviews Neuroscience. 7(11), 860-72 (2006).
Schwartz SD, Hubschman JP, Heilwell G, Franco-Cardenas V, Pan CK, e. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet. 379(9817), 713-20 (2012).
Weiland JD, Cho AK, Humayun MS. Retinal prostheses: current clinical results and future needs. Ophthalmology. 118(11), 2227-37 (2011).
Wong WL, Su X, Li X, Cheung C, Klein R, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. The Lancet Global Health. 2 (2) e106-e116 (2014).
Also In Vision
Trending
Popular articles on BrainFacts.org